Hospital Medicine: Clinical
Hospital Medicine 7
770 - Evaluating the Safety of Avoiding Lumbar Punctures in the Management of Low-risk Febrile Infants 7-28 Days Old
Publication Number: 770.416

Ammar Kamil, MD, FAAP (he/him/his)
Pediatric Hospital Medicine Fellow
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background:
The clinical evaluation of febrile infants has been extensively studied with the aim to improve the sensitivity in identifying infants at risk for invasive bacterial infections while decreasing the harm of unnecessary invasive procedures. In 2018, our institution implemented a clinical pathway for febrile infants 7-28 days utilizing a new risk stratification protocol limiting lumbar punctures (LP) in those classified as low-risk.
Objective:
To evaluate the number of safely avoided LPs and the incidence of missed cases of meningitis.
Design/Methods:
We performed a retrospective study of full-term infants aged 7-28 days who presented to the emergency department between 2018-2022 for fever and managed on the febrile infant clinical pathway. Patients were identified utilizing ICD-10 codes for fever, bacteremia, urinary tract infection, pyelonephritis, and meningitis. Data collected included demographics, bacterial cultures results, and LP procedures. Infants who presented as ill-appearing, with signs of focal infection, or with seizure were excluded. Per the pathway, infants were classified as low-risk if they did not have any of the following criteria: history of prolonged hospitalization, prolonged newborn nursery course or history of unexplained hyperbilirubinemia, complete blood cell count (CBC) with white blood cell count (WBC) < 5000/cc or >15000/cc or >1500/cc bands, positive urinalysis (UA) for nitrites, leukocyte esterase or WBC >5/HPF, procalcitonin >1 ng/ml. If an infant met criteria for low-risk, only CBC, procalcitonin, blood culture, UA, and urine cultures were recommended but LP and antibiotics were not required. Descriptive statistical analysis was used to analyze the data.
Results:
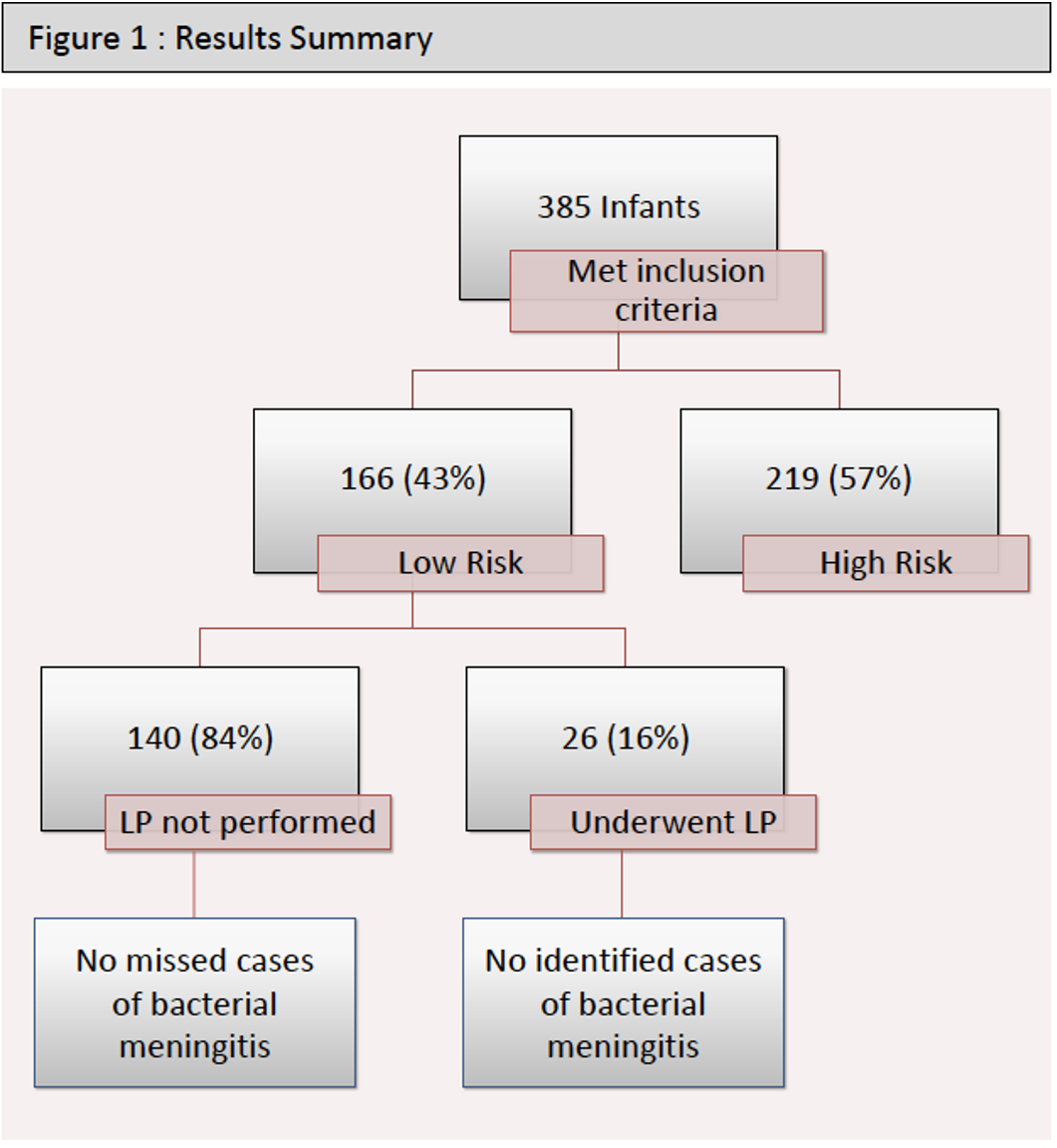
385 infants met inclusion criteria;166 (43%) were classified as low-risk and 219 (57%) were high-risk. Of those 166 low-risk infants, 140 did not undergo LPs. However, 26 of the 166 low-risk infants who could have avoided LPs per our clinical pathway, did undergo a LP: 13 had LP performed at another institution prior to transfer; 7 were done in our ED based on clinicians’ judgment, 4 were performed after admission due to positive blood and/or urine cultures; 1 performed for increasing fussiness; and 1 for development of seizures. Of the 140 low-risk infants that did not undergo a LP, there were no cases of missed meningitis. Of those who had a LP, none were found to have bacterial meningitis, but one case of viral meningitis was detected.
Conclusion(s):
Based on our institution’s stratification criteria, LPs were safely avoided in low-risk febrile infants 7-28 days without missing any cases of bacterial meningitis.