Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 3
649 - Telemedicine Use Among Pediatric Asthma Patients in the Era of COVID-19 in an Academic Healthcare System
Publication Number: 649.456

Kaitlin M. Hall, MD, MPH (she/her/hers)
Health Services Research Fellow/General Pediatrician
University of California, Los Angeles David Geffen School of Medicine
Los Angeles, New York, United States
Presenting Author(s)
Background:
Environmental, and social factors can cause persistent inequities in access to care and asthma outcomes among children from lower socioeconomic statuses and historically marginalized racial and ethnic groups. Innovative approaches for asthma are needed. We hypothesize that telemedicine, which expanded rapidly during the COVID-19 pandemic, may be a promising approach to increase access to asthma care for historically marginalized children.
Objective:
We describe characteristics of pediatric asthma telemedicine users and characterize trends of use throughout the COVID-19 pandemic at a large academic medical center.
Design/Methods:
We conducted a retrospective analysis of electronic health record data across UCLA Health from March 2019 (approximately 1-year prior to the start of the pandemic) to March 2022 to describe (a) telemedicine user characteristics including age, gender, race and ethnicity, preferred language, asthma severity, comorbidities, insurance type, and social vulnerability index (SVI) quartile and (b) trends of asthma-related telemedicine use over time. We used multivariable regression to evaluate the relationship between patient sociodemographics and occurrence of a telemedicine visit for asthma.
Results:
The percentage of telemedicine visits reached a peak early in the pandemic (April 2020), comprising 74.3% of all visits, and decreased to 13.6% in March 2022 (Figure 1). Compared to NH white patients, NH Black patients had 51% lower odds of having a telemedicine visit for asthma (95% CI: [0.28, 0.85], p=0.02), while NH Asian patients had 52% higher odds (95% CI: [1.07, 2.16], p=0.02), and Hispanic/Latine patients had 23% higher odds (95% CI: [0.92, 1.64], p=0.22). Patients with severe persistent asthma (OR 2.36, 95% CI: [1.40, 3.97], p=0.001) had higher odds of a telemedicine visit for asthma (Table 2). Insurance type and SVI quartiles generally did not yield significant differences in visit type (telemedicine vs. in-person).
Conclusion(s):
The proportion of telemedicine visits for asthma rapidly increased early in the COVID-19 pandemic and did not decline to pre-pandemic levels. Patients with more severe asthma had higher odds of having a telemedicine visit, and though NH Black patients had lower odds of having a telemedicine visit, NH Asian and Hispanic/Latine patients both had higher odds. There was no significant difference between insurance types or those with more social vulnerability (SVI quartile 3 or 4) in odds of having a telemedicine visit. Telemedicine appears to increase access for some groups, but may not be an equitable increase.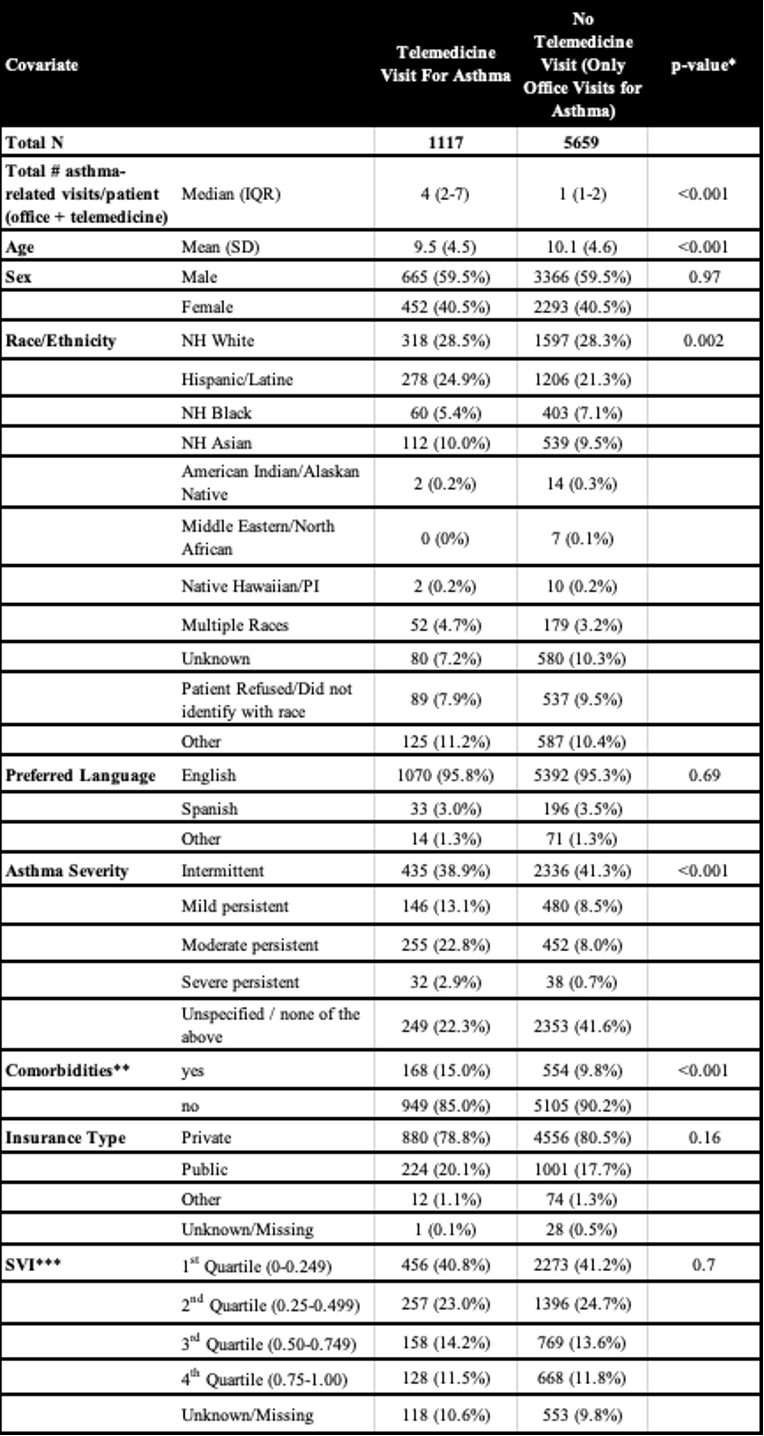
.png)
.png)

