Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 5
124 - Patent ductus arteriosus shunt duration and severity, defined by echocardiography and association with development of severe retinopathy of prematurity in extremely preterm born infants
Publication Number: 124.427
- AG
Anna Gudmundsdottir, MD (she/her/hers)
Consulting neonatologist and Postdoc
Karolinska Institutet
Solna, Stockholms Lan, Sweden
Presenting Author(s)
Background:
Conservative patent ductus arteriosus (PDA) treatment can expose the extremely preterm (EPT) infant to a long duration of PDA shunt which has been associated with risk of neonatal morbidities.
Objective:
This study investigated the association of PDA shunt duration and severity on the development of severe ROP in the EPT.
Design/Methods:
In this Swedish cohort study, prospectively collected data was used, from a cohort of EPT infants born 2017-19 (n=206) previously enrolled in a randomized-controlled trial of fatty acid supplementation. PDA shunt duration and significance were retrospectively defined into mild vs moderate and severe according to echocardiography criteria suggested in the PDA-Tolerate trial by Clyman et al 2019. We studied the association of the exposures, total shunt duration in days and days with a moderate to severe shunt, with severe ROP both descriptively and with logistic regression.
Results:
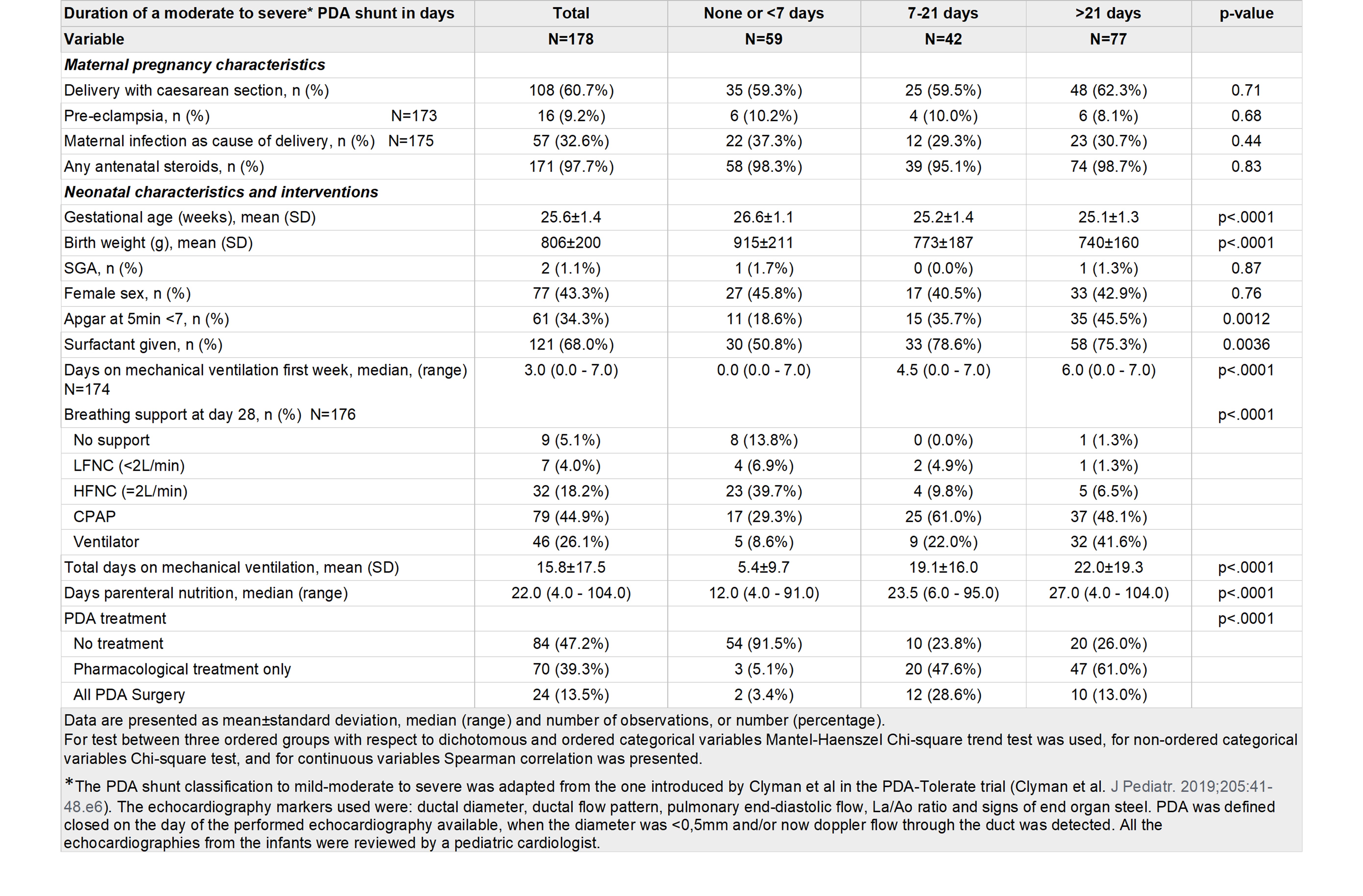
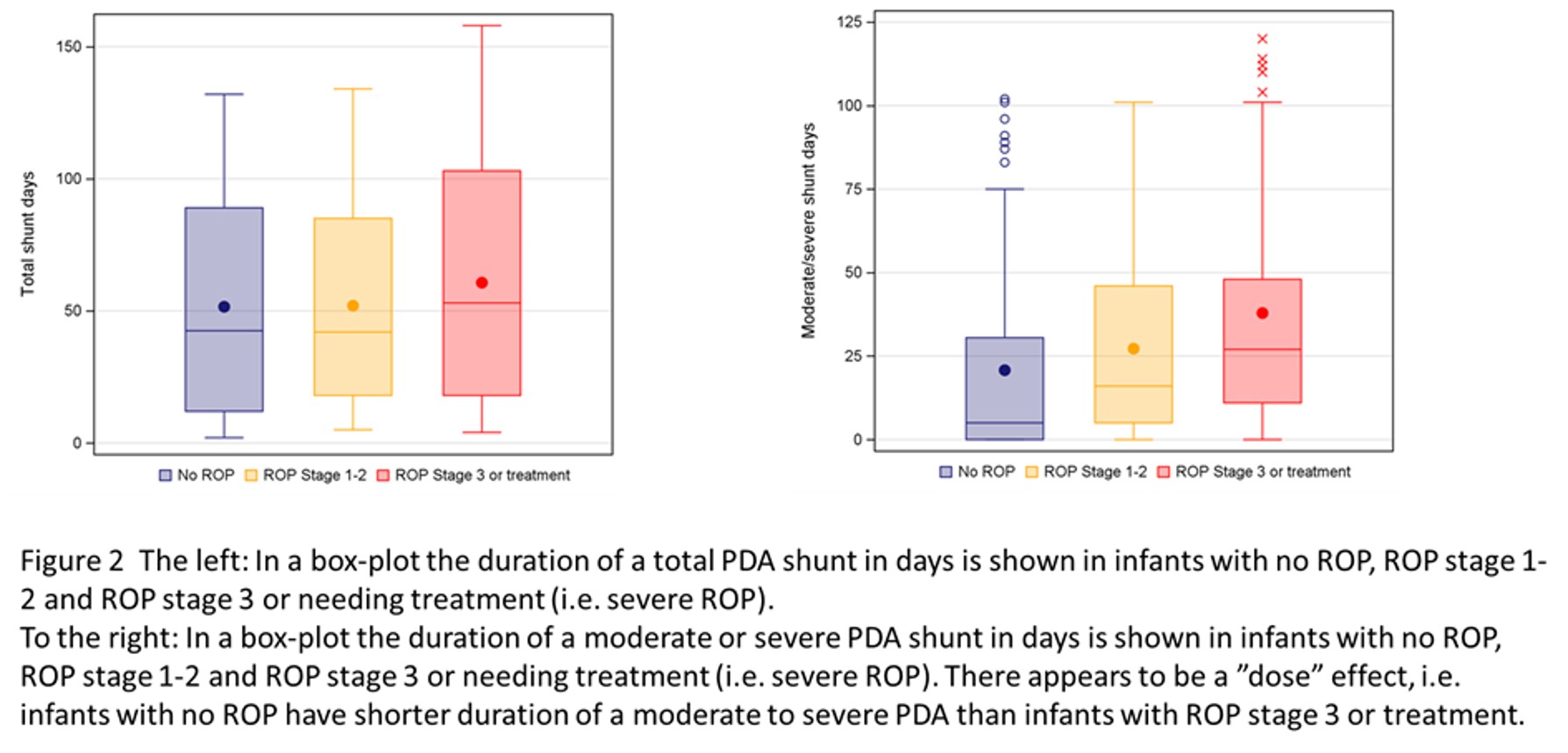
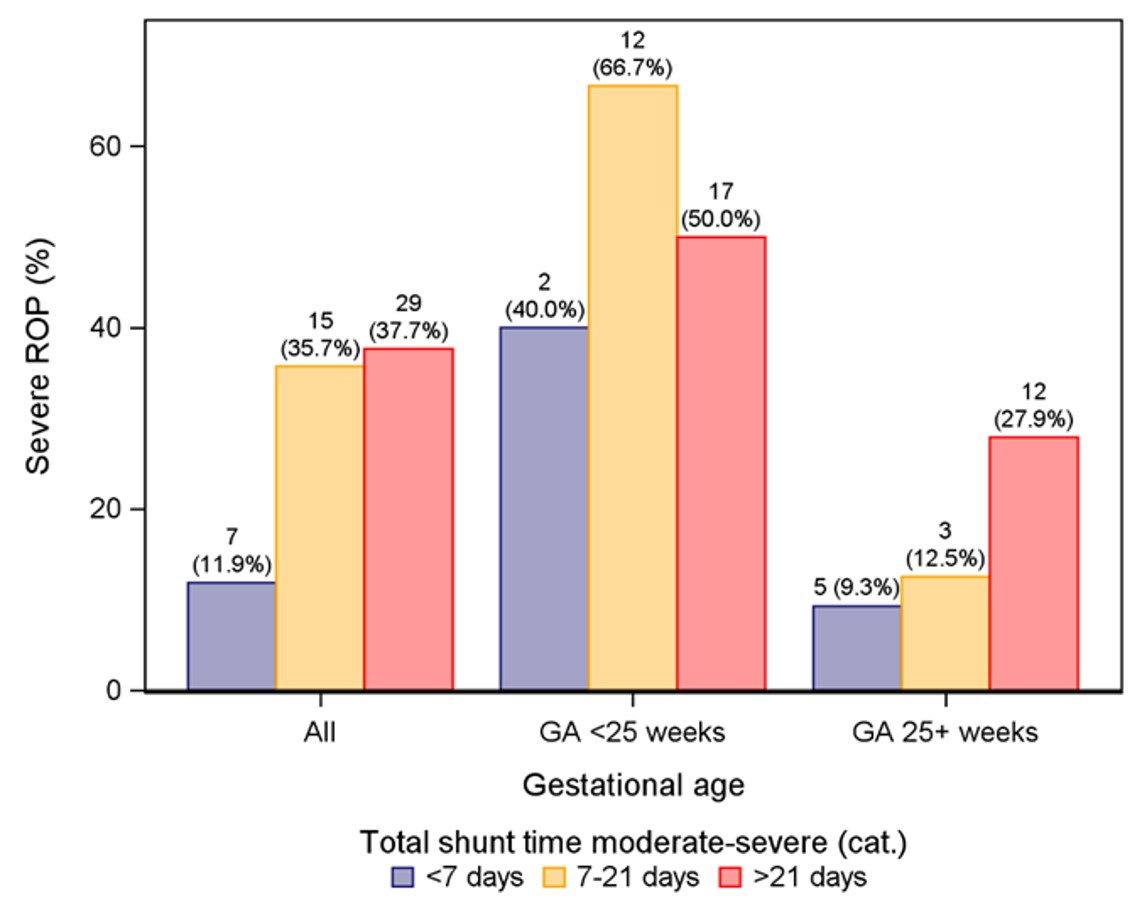
178 infants survived to term age, 84 (47%) received no PDA treatment, 70 (39%) were treated only pharmacologically and 24 (14%) surgically, either after prior pharmacological treatment or not. The mean start of pharmacological treatment was 9.3 days +/- 5.4. 13 infants (7%) had a total shunt duration of < 7 days, 39 (22%) of 7-21 days and 126 (71%) of >21 days. In figure 1, infant characteristics are shown by the duration of a moderate to severe shunt. Figure 2 displays shunt duration and development of different stages of ROP. In a crude logistic regression model, the per-week increase of total shunt duration was not significantly associated with severe ROP, whereas the crude odds ratio (OR) was 1.10 95% CI 1.02-1.18, per 1 week increase for the duration of moderate to severe shunt. In figure 3, the proportion of infants with severe ROP are shown by gestational age (GA) categories and a moderate-severe PDA shunt duration. The crude OR for the comparison of a shunt duration < 7 days vs ≥7 days was 4.36 95% CI 1.82-10.42 but after preliminary adjustments with GA, birth weight and randomized treatment group, the association was not statistically significant, adjusted OR 2.06 95% CI 0.74-5.76. Further adjustment analysis including exploring echocardiography markers is ongoing.
Conclusion(s):
The majority of EPT infants were exposed to a duration of PDA shunt > 3 weeks. Shunt duration through PDA alone was not associated with severe ROP, but duration of a shunt with moderate to severe significance was. Understanding the associations of PDA shunt severity and duration with neonatal morbidities such as ROP are important when PDA treatment strategies are defined and tested.