Emergency Medicine: All Areas
Emergency Medicine 13
367 - PEM Fellowship Director National Intimate Partner Violence Survey of Fellow Experience
Publication Number: 367.404

Marci Fornari, MD (she/her/hers)
Pediatric Emergency Medicine Attending
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background:
1 in 3 women and 1 in 4 men have experienced intimate partner violence (IPV) within their lifetime. The American Academy of Pediatrics recommends that pediatricians routinely screen caregivers for IPV and that pediatric training programs incorporate IPV into their curricula. Despite this, nearly two-thirds of practicing pediatricians report they did not receive IPV training during residency. Few published studies have addressed IPV education in general pediatric training programs and there are no studies addressing IPV education within pediatric emergency medicine (PEM) training programs. This is particularly important as PEM physicians are in a unique position to recognize and support IPV survivors and their families.
Objective:
1. Describe the IPV education PEM fellows experience during training.
2. Understand the perceived barriers to IPV education during PEM fellowship.
Design/Methods:
We distributed a REDCap survey through the PEM fellowship director listserv (n=86 programs). Survey domains included IPV screening practices within pediatric emergency departments and PEM fellowship IPV education. Frequencies of responses were calculated.
Results:
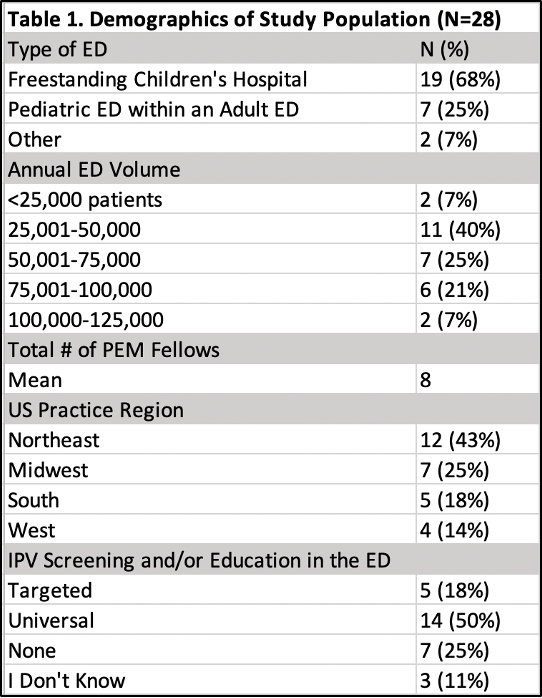
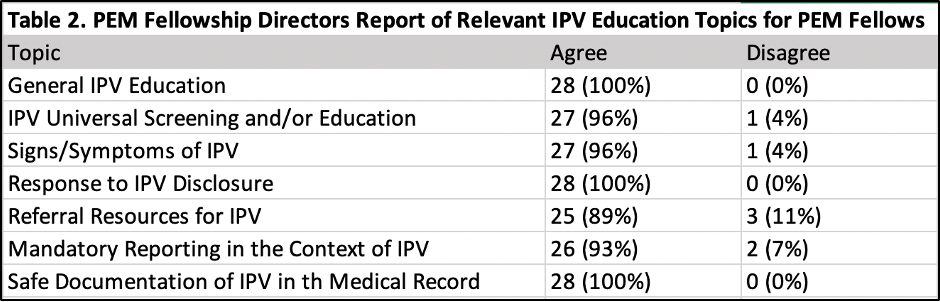
28 fellowship directors (33% response rate) participated; table 1 presents demographics. Only 21% of fellowship directors reported formal IPV education is a component of the fellowship curriculum. Of the fellowship programs providing IPV education, the majority educate on referral resources (83%) and signs and symptoms of IPV (67%) via synchronous lectures (83%) on an annual basis (83%). Less common topics included universal screening (33%), response to IPV disclosure (33%), mandatory reporting in the context of IPV (33%), and safe documentation in the medical record (50%). All study respondents agreed that education regarding IPV should be included in the PEM fellowship curriculum (Table 2). The majority expressed that the material should be delivered via online learning (61%) and/or synchronous lectures (57%) on an annual basis (61%). The most commonly reported barriers to providing IPV education were time (82%) and lack of content experts (79%).
Conclusion(s):
PEM program directors agreed that fellowship training should include IPV education but almost 4 in 5 programs in our sample do not provide any formal IPV education for their fellows. Further, training content was quite limited. Thus, PEM fellows would benefit from a formalized and more robust IPV curriculum to enhance their training.