Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 8
566 - Health Inequities in Antibiotic Choice for Common Infections in Pediatric Emergency Departments Despite Antimicrobial Stewardship Initiatives
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 566
Publication Number: 566.412
Publication Number: 566.412
Zuri Hudson, Children's Mercy Hospital, Sharpsburg, GA, United States; Zuri Hudson, Children's Mercy Hospitals and Clinics, Sharpsburg, GA, United States; Brian R. Lee, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Elizabeth Monsees, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Amanda Nedved, Children's Mercy Hospitals and Clinics, Lenexa, KS, United States; Frances Turcotte Benedict, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States; Rana E. El Feghaly, Children's Mercy Kansas City, Kansas City, MO, United States

Zuri Hudson, DO (she/her/hers)
Chief Resident
Children's Mercy Hospital
Sharpsburg, Georgia, United States
Presenting Author(s)
Background: Health inequity in antibiotic prescribing for common pediatric infections has been described, including in our institution.
Objective: To evaluate the impact of an antimicrobial stewardship program (ASP) on health inequity in relation to appropriate antibiotic prescribing for common infections in the Emergency Department (ED).
Design/Methods: We reviewed all encounters from 2 freestanding EDs within our institution of patients 2 months - 18 years old with diagnoses of acute otitis media, community acquired pneumonia, group A streptococcal pharyngitis, skin and soft tissue infections, and urinary tract infections who were prescribed systemic antibiotics. We analyzed use of first-line agent as recommended by national guidelines. Our outpatient ASP team applied initiatives aligned with the Center for Disease Control and Prevention (CDC) core elements starting in August 2018 with improvement in antibiotic use overall. We compared the baseline period (July 2017 - July 2018) to the post-implementation period (August 2018 -December 2020) to determine whether there is health inequity in antibiotic prescribing. A multivariable regression analysis calculated the odds ratio of appropriate antibiotic choice stratified by gender, age, race/ethnicity, and insurance type in both periods.
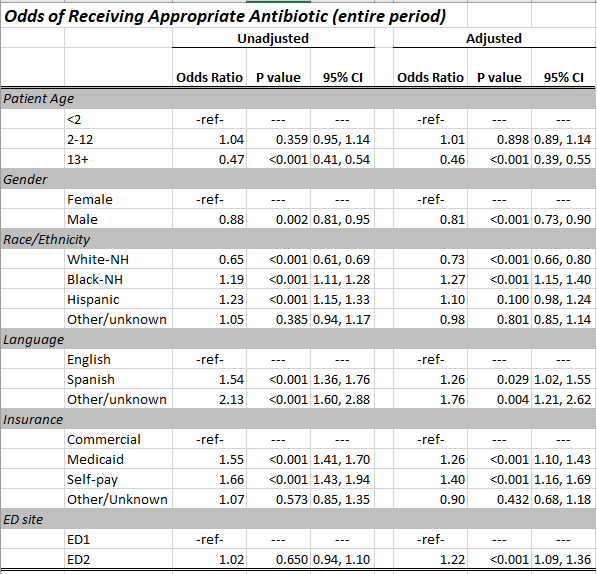
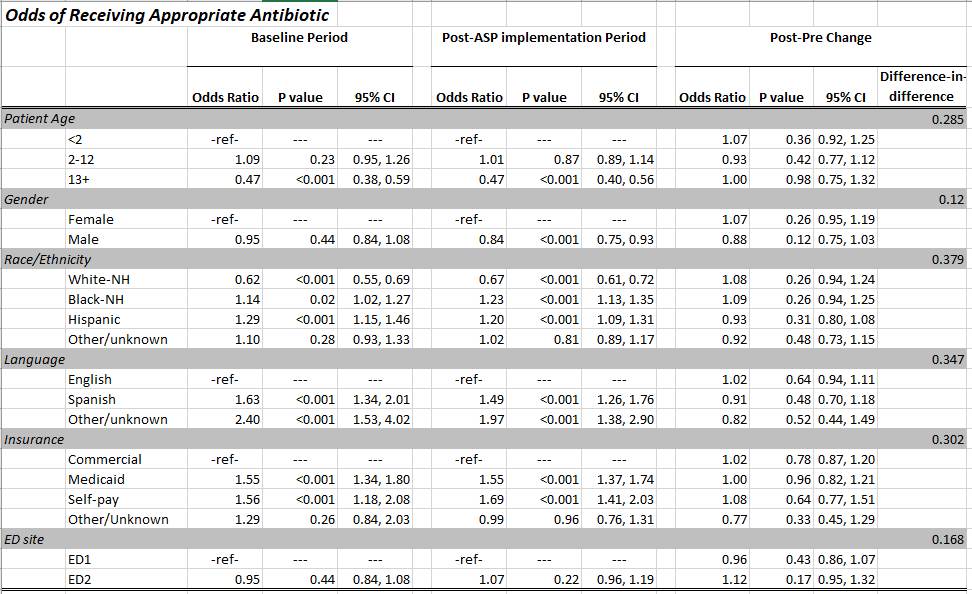
Results: We evaluated 14,329 total encounters (5,731 baseline, 8,598 post-implementation). Demographic factors were similar amongst both periods. Throughout our analysis period, White non-Hispanic (NH) children, those ≥ 13 years old, those with preferred language other than English, and those with commercial insurance were less likely to receive the recommended first line treatment for all diagnosis (Table 1). The differences between the sociodemographic subsets persisted despite our ASP efforts; additionally, in the post-implementation period, we saw a gender inequity with males being less likely to be prescribed appropriate antibiotics compared to females (Table 2).
Conclusion(s): Despite nationally recommended guidelines for antibiotics based on diagnoses and antibiotic stewardship initiatives, there continue to be inequities in first-line antibiotic prescribing in our ED. Leaders within antimicrobial stewardship should consider drivers of health inequity when developing improvement initiatives. Our next step is to explore clinician perspectives related to socioeconomic variables in prescribing for common infections in the ED and develop ASP initiatives specifically targeting health inequities.