Infectious Diseases
Infectious Diseases 5
434 - Human Parechovirus (HPeV) Infection in Infants Under 3 Months of Age 2018-2022
Publication Number: 434.419
Avni Sheth, DO (she/her/hers)
Resident Physician
Goryeb Children's Hospital
Morristown, New Jersey, United States
Presenting Author(s)
Background:
HPeV typically causes self-limiting respiratory and gastrointestinal infections, however, in infants it can cause a severe sepsis-like illness and CNS disease. HPeV subtype A-3 is associated with severe disease. In July 2022, the CDC issued a health advisory regarding increased reports of HPeV in the US.
Objective:
Our objective was to evaluate the epidemiology of HPeV meningitis at Atlantic Health System before and after the 2022 surge.
Design/Methods:
A retrospective study was conducted via review of the electronic health record of infants less than 90 days of age with HPeV meningitis admitted from 01/01/18-12/31/21 (Group 1) and 01/01/22-10/31/22 (Group 2). HPeV meningitis cases were identified by positive CSF testing with the FilmArray meningitis/encephalitis panel (BioFire Diagnostics, Salt Lake City, UT). Data was entered in REDCap. The differences between the two group of patients in clinical data and laboratory values were analyzed by Student’s t test and x2, were appropriate. Statistical significance was assumed for p< 0.05.
Results:
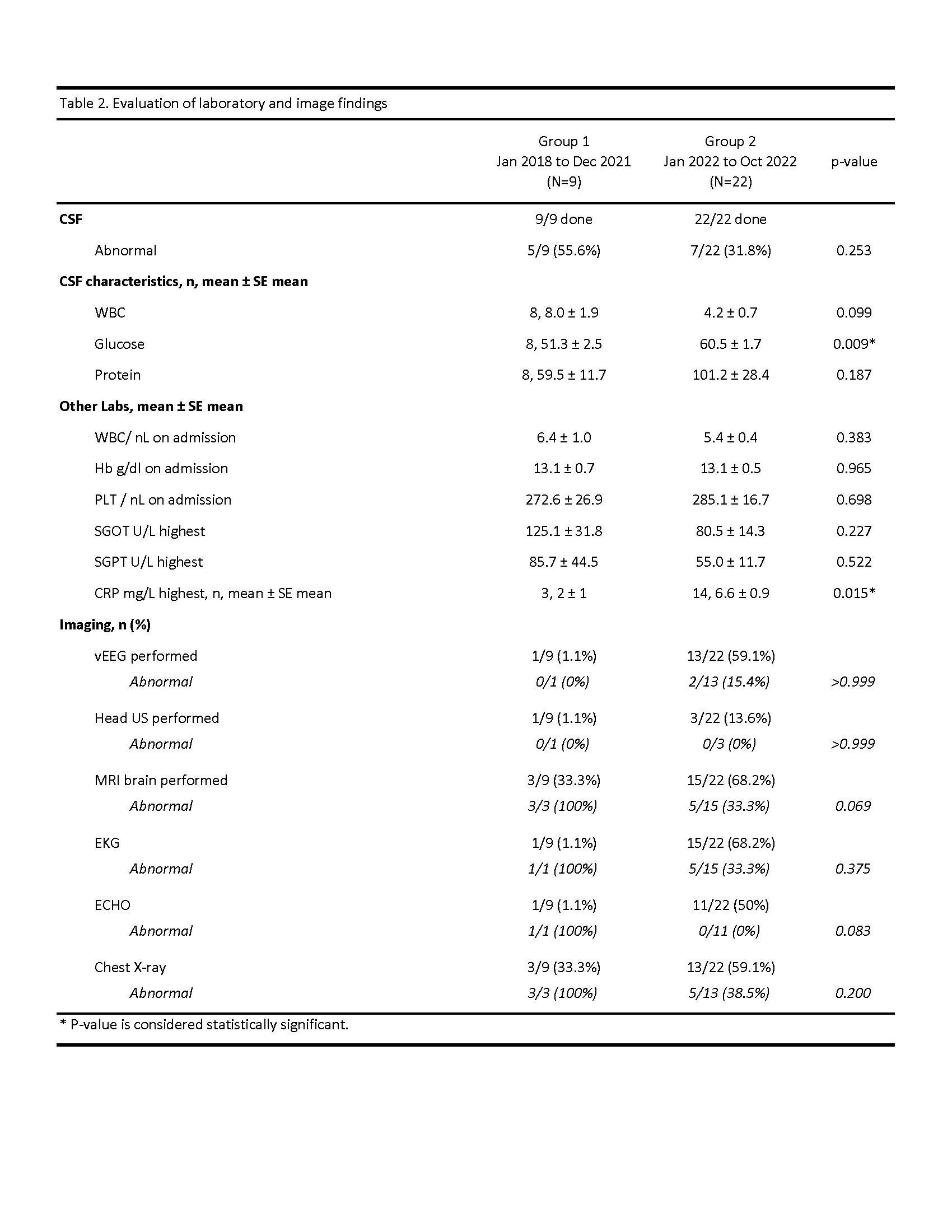
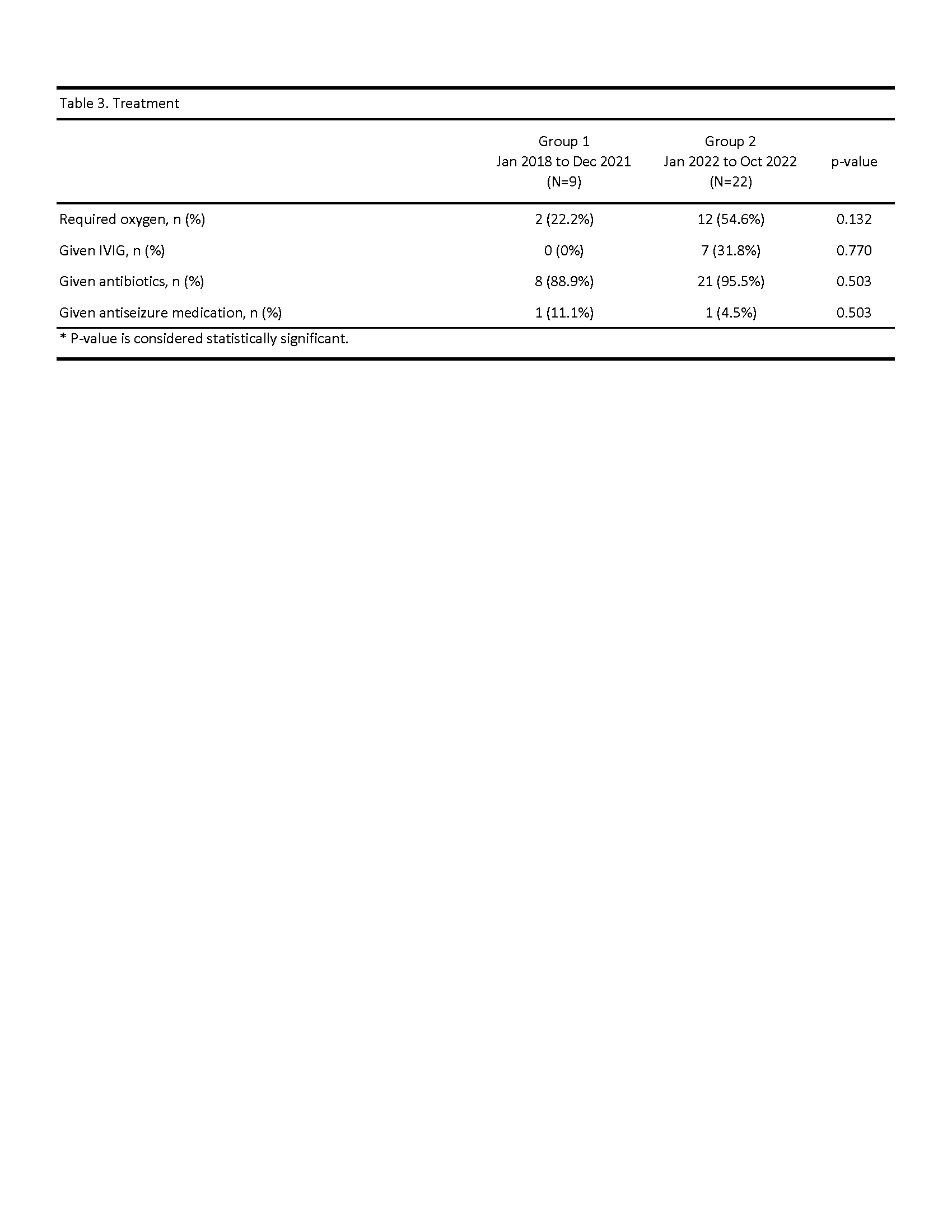
Table 1 depicts the demographic and baseline clinical characteristics of both cohorts. Infants admitted in 2022 had a statistically significant longer length of stay when compared with Group 1. Fever, GI symptoms, and irritability were the most common presenting symptoms. Most infants had normal inflammatory markers and CSF indexes with minor differences between CSF glycorrhachia and CRP values among cohorts (Table 2). Infants in Group 1 had a higher rate of abnormal findings in MRI, EKG, echocardiogram, and CXR. One third of patients in Group 2 were treated with IVIG whereas no patients in Group 1 (Table 3). Follow up for both cohorts of patients show neurodevelopmental delays in about one tenth of the populations. No deaths were recorded.
Conclusion(s):
An increase in infants with HPeV meningitis was seen in 2022 compared to other years. The presentation and clinical course of infants in the two groups were not dramatically different although there was a larger percentage of abnormalities seen in infants with MRI performed in Group 1. In infants with HPeV meningitis, white matter abnormalities on MRI and neurodevelopmental sequelae are reported which warrant further longitudinal follow-up..png)