Hospital Medicine: Clinical
Hospital Medicine 7
772 - Feasibility of a Contraception Intervention for Hospitalized Adolescents and Young Adults
Publication Number: 772.416

Abbey Masonbrink, MD MPH (she/her/hers)
Associate Professor of Pediatrics
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background:
Unintended pregnancy in adolescents and young adults (AYAs) is linked with negative outcomes.
Objective: We sought to evaluate the feasibility, acceptability and preliminary efficacy of a contraception intervention in the pediatric hospital.
Design/Methods:
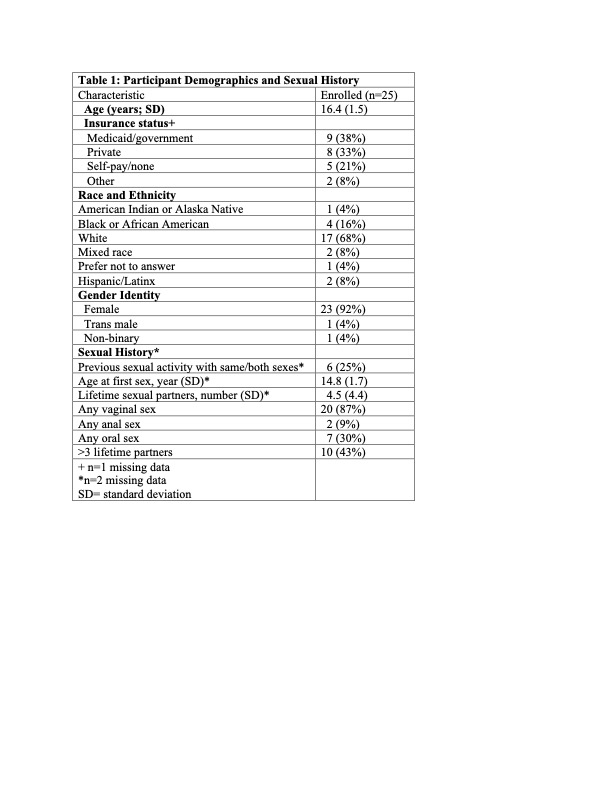
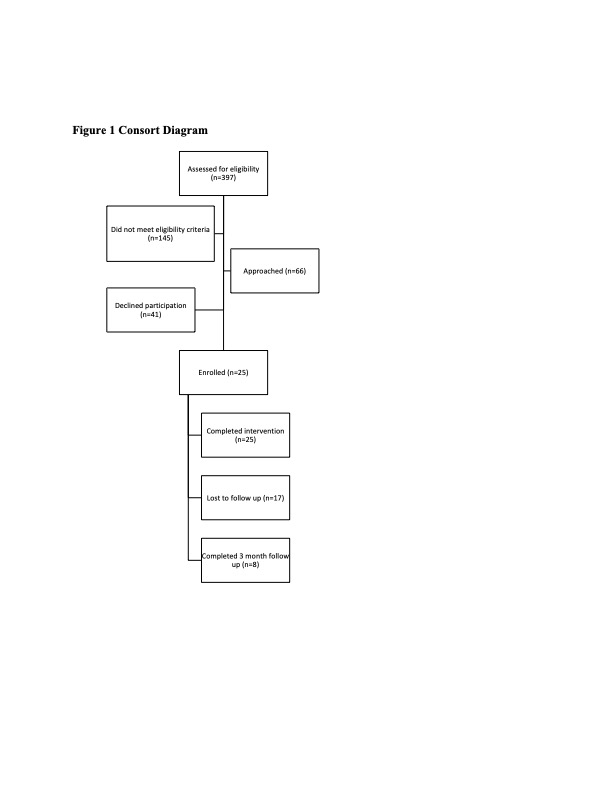
We conducted a pilot study of hospitalized AYA females aged 14-21 years who reported past or anticipated sexual activity. A health educator offered a tablet-based intervention to explore family planning goals and offer contraception education and initiation. Medications were reviewed and prescribed by study physicians, if desired. We assessed demographics, sexual health behaviors, and teratogen exposure. We assessed intervention feasibility (i.e., intervention completion, duration, disruption to care); acceptability (i.e., proportion rating as acceptable/satisfactory) among AYAs, parents/guardians, and healthcare providers; and preliminary efficacy (e.g., contraception uptake).
Results:
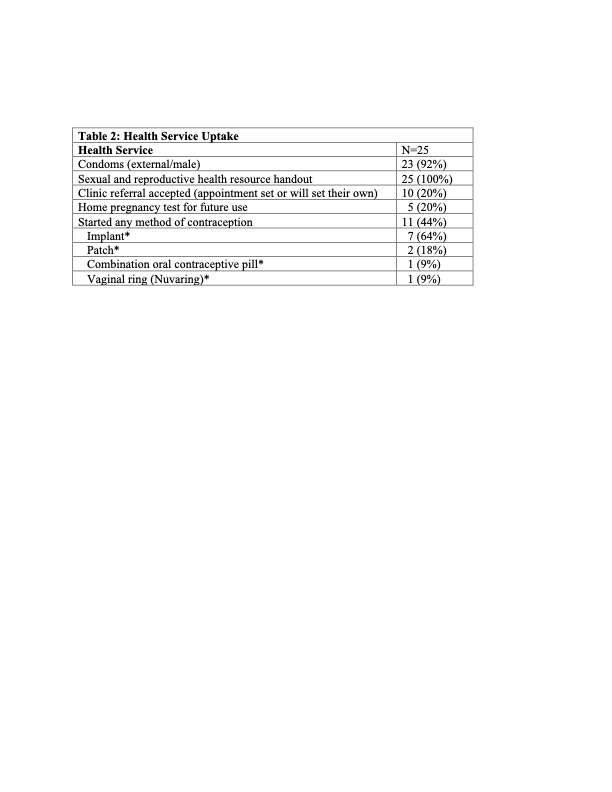
We enrolled 25 participants, most (n=15, 60%) of which were “trying to avoid pregnancy.” Five participants (20%) were using a hormonal birth control method (all using oral contraceptive pills [OCPs]). Eight (32%) participants were taking teratogenic medication but only three (38%) reported being informed the medication was potentially harmful. The intervention demonstrated high feasibility as all enrolled participants (n=25, 100%) completed the intervention and median intervention duration was 32 (IQR 25-45) minutes. Among eleven nurses, 82% (n=9) reported the intervention was not at all/minimally disruptive to their workflow. All AYAs were very/somewhat satisfied with the intervention and 88% (n=7) of eight parents/guardians surveyed felt it was acceptable for the educator to meet privately with their child. For preliminary efficacy, twenty-three participants (92%) received condoms and eleven (44%) started or changed contraception methods during their hospitalization (Table 2). Of those starting contraception, seven (64%) started the subdermal implant, two (18%) started the patch, one (9%) chose the OCP, and one (9%) started the vaginal ring.
Conclusion(s):
Our findings support the feasibility and acceptability of our contraception intervention in the pediatric hospital. Nearly half of AYA participants receiving contraception; of those nearly two-thirds chose the subdermal implant. Efforts to expand contraception access are critically important to reduce unintended pregnancy, especially as restrictions to reproductive health care, including abortion, are increasing.