Critical Care
Critical Care 4
729 - Magnesium and High Flow Nasal Cannula Adjunct Protocols for an Established Asthma Pathway
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 729
Publication Number: 729.401
Publication Number: 729.401
Jennifer Biber, Akron Children's Hospital, Akron, OH, United States; Kailey A. Remien, Akron Children's Hospital, akron, OH, United States; Christopher Page-Goertz, Akron Children's Hospital, Hudson, OH, United States; Samantha Gunkelman, Akron Children's Hospital, Akron, OH, United States; Jonathan H. Pelletier, Akron Children's Hospital, Akron, OH, United States

Kailey A. Remien, DO (she/her/hers)
Pediatric Resident
Akron Children's Hospital
Akron, Ohio, United States
Kailey A. Remien, DO (she/her/hers)
Pediatric Resident
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
First Author(s)
Background: Our institution initiated a respiratory therapist (RT) and nursing driven asthma pathway (AP) on the acute care wards and the PICU in 2009. This pathway has now been extended to include several emergency departments and inpatient units. Implementation of the asthma pathway led to a reduction of hospital LOS and PICU LOS, total charged items per patient, and a reduction in the cost of hospitalization. Those requiring IV bronchodilators or high flow nasal cannula (HFNC) did not qualify for the AP, and were treated “off-pathway.” Increasing the number of patients "on-pathway" improves standardization and reduces complications and waste. No published APs include HFNC or magnesium drips, making this a novel pathway.
Objective: The objective of this study was to increase standardization by including more patients on the AP without increasing PICU LOS or time to every two-hour albuterol treatments (Q2hour). (SMART
Aim: increase the number of patients on pathway by 10% in 1 year).
Design/Methods: A multidisciplinary team including RTs, nurses, physicians, and advanced practice providers was assembled to develop the adjunct algorithms and gather feedback. Utilizing the Model for Improvement, the team tested these pathways on 15 patients as the first PDSA cycle from 10/1/21 to 3/28/22. Minor edits were made to the algorithms which were finalized 3/28/22. The second cycle was then started and expanded to all the ordering providers in the PICU. This cycle ran from 3/28/22 to 12/11/22 with a total of 101 encounters.
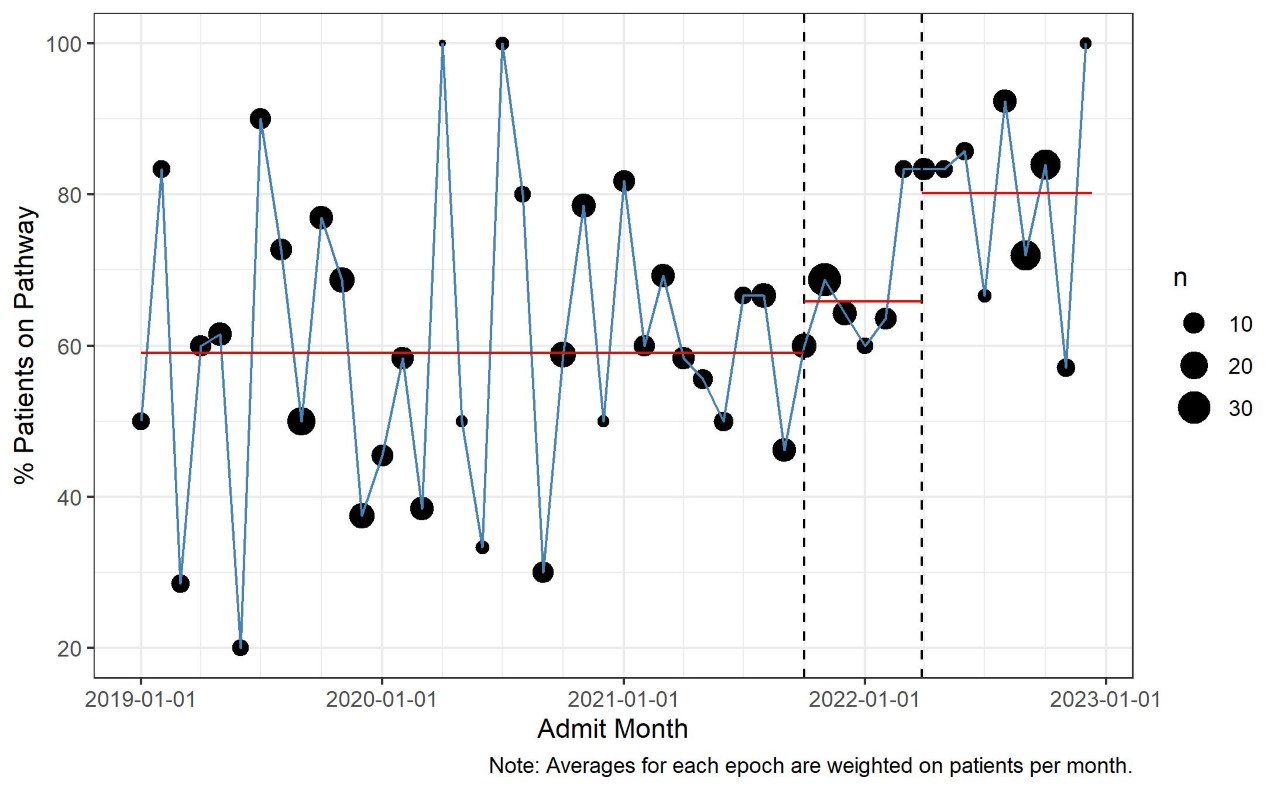
Results: The number of patients on pathway increased from 59.1% (192/325) before 10/01/2021 to 80.2% (81/101) after 3/28/2022 (p < 0.001). There was no significant change in time to every two-hour albuterol administration (5.6 [2.6-12.7] versus 7.4 [2.5-15.4] hours, p = 0.54), PICU length of stay (18.7 [12.5-28.5] versus 19.1 [12.4-29.2] hours, p = 0.78) or standardized unit cost ($8,876 [$6,109-$12-213] versus $9,295 [$5,946-$12,091], p = 0.85).
Conclusion(s): These nursing/RT run HFNC and magnesium drip adjunct asthma pathways increased the proportion of included PICU patients. Improvement in care standardization was not associated with significant changes in duration of therapy, PICU length of stay, or standardized unit cost. Having more patients on AP may allow for refinement and improvement in care of these patients.