Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 6
466 - Incidence of Sepsis and the Outcomes of Antibiotic use in VLBW Infants at a High-risk, Inner City, Level III Neonatal Intensive Care Unit.
Publication Number: 466.432
.jpg)
Sheetal Sriraman, MD (she/her/hers)
Pediatric Resident Physician
SUNY Downstate Health Sciences University
Brooklyn, New York, United States
Presenting Author(s)
Background: Neonatal sepsis is associated with increased morbidity and mortality rates in neonates. Studies show that antibiotic use trends are center-dependent and are most influenced by the incidence of sepsis in the unit and the risk factors for sepsis in the population.
Objective:
To analyze the incidence of neonatal sepsis and the outcomes of antibiotic use in very low birth weight (VLBW) infants at a high-risk inner-city level III neonatal intensive care unit in an African- and Caribbean-American inner-city population.
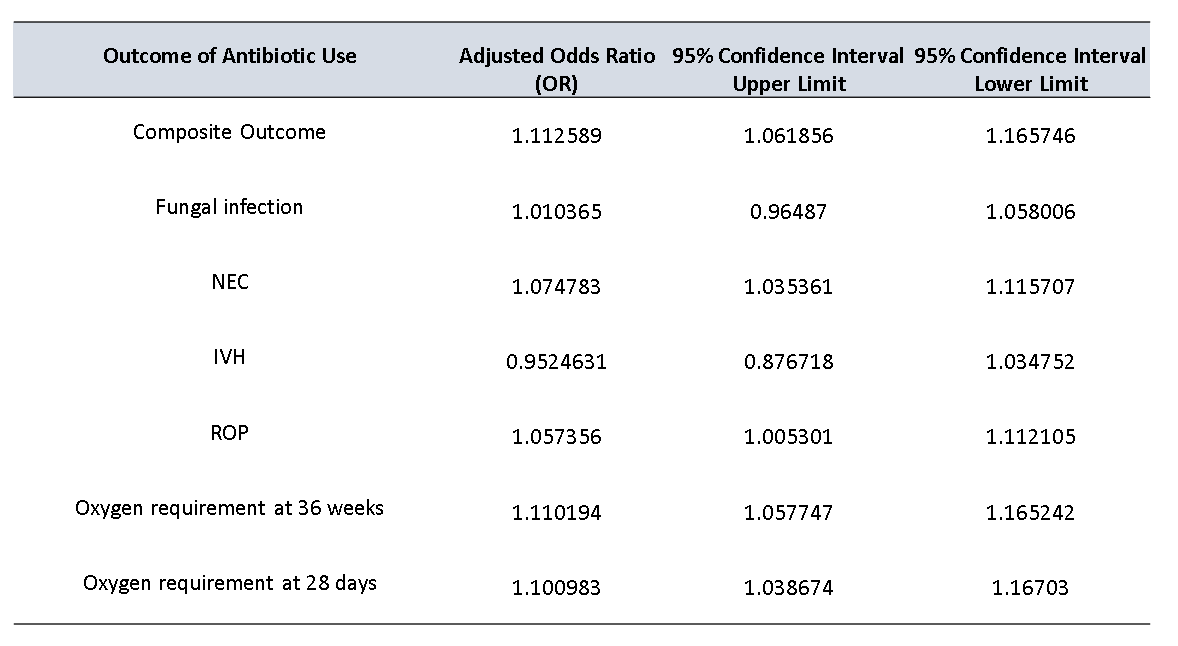
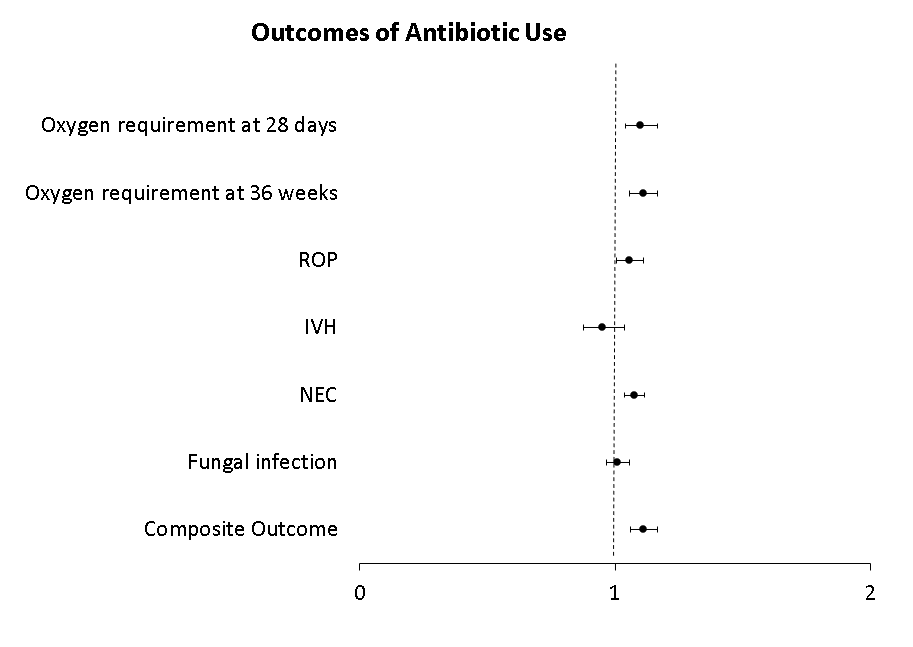
Design/Methods: We conducted a cross-sectional retrospective chart review from 2016 to 2022 in a level III neonatal unit. We included all neonates weighing less than 1500 g at birth during this period without congenital anomalies who lived past 24 hours. Early onset sepsis (EOS) and late-onset sepsis (LOS) were defined as culture-proven blood or CSF infection within or after the first three days of life respectively. The composite outcome was defined as the incidence of necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP), interventricular hemorrhage (IVH), or oxygen requirement at 36 weeks postmenstrual age. Descriptive statistics were used to describe the prevalence of EOS and LOS. Logistic regression was used to analyze the association between antibiotic use and outcome, after correcting for potential confounders such as gestational age, SNAPPE II score, and birth weight. The adjusted odds ratios (OR) with a 95% confidence interval (CI) were described.
Results:
A total of 198 infants were identified out of which the incidence of EOS, LOS, and fungemia was 1.5% (3/198), 9.6% (19/198), and 3% (6/198) respectively. The mean duration of antibiotics was 4 days for EOS and 17 days for the entire NICU admission. The mean gestational age was 28 4/7 weeks (75% CI: 28 0/7-29 1/7). The mean birth weight was 1048 g (75% CI: 1021-1074). Intra-amniotic infection was seen in 31% (56/177). We found an association between the duration of antibiotic use and the composite outcome, NEC, ROP, and oxygen requirement at 36 weeks post-menstrual age with an adjusted odds ratio of 1.11 (95% CI 1.06-1.16), 1.07, 95% CI 1.03-1.115), 1.05. 95% CI 1.005-1.112), and 1.11, 95% CI 1.05-1.16) respectively. (Fig 1 and 2)
Conclusion(s): Increased duration of antibiotic use showed a trend of increased incidence of the composite outcome, NEC, ROP, and oxygen requirement at 36 weeks. NICU-specific antimicrobial stewardship programs can play a significant role in reducing the rate and duration of antibiotic use. Further studies including a larger number of LBW infants are needed to increase the power of the study.