Emergency Medicine: All Areas
Emergency Medicine 13
358 - Comparing pediatric blunt head trauma prediction tools and factors associated with deviation of their use
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 358
Publication Number: 358.404
Publication Number: 358.404
Cheuk Kwok, Orlando Health, Orlando, FL, United States; Shaye Busse, University of Central Florida College of Medicine, Orlando, FL, United States; Jamie Marliere, University of Central Florida College of Medicine, Loma Linda University Emergency Medicine Residency, Loma Linda, CA, United States; April N. Taniguchi, University of Central Florida College of Medicine, Charleston, SC, United States; Kamal Chavda, University of Central Florida College of Medicine, Orlando, FL, United States; Andrea Rivera-Sepulveda, Nemours Children's Hospital, Orlando, FL, United States

Andrea Rivera-Sepulveda, MD, MSc
Physician
Nemours Children's Hospital
Orlando, Florida, United States
Presenting Author(s)
Background: Head injuries are a common cause of emergency department (ED) visits and hospitalizations in pediatric patients. Prediction tools have been developed to aid in the clinical decision of ruling out the presence of traumatic brain injury, in order to decrease exposure to radiation. However, a third of pediatric head injuries continue to receive neuroimaging. The literature on the factors that affect deviation from prediction tool recommendations against the use of head computed tomography (CT) is limited.
Objective: The objective of this study is to compare prediction tools and the factors associated with deviation from recommendations.
Design/Methods: Retrospective cohort study of patients 0 to 18 years who visited the pediatric ED with a chief complaint of head injury in 2019. Data included ED visit metrics, characteristics of the injury, head CT recommendations by a best practice advisory (BPA) and Pediatric Emergency Care Applied Research Network (PECARN), head CT use, and traumatic brain injury (TBI) presence. Chi-squared, Fisher’s exact test, and odd ratio were used, as appropriate.
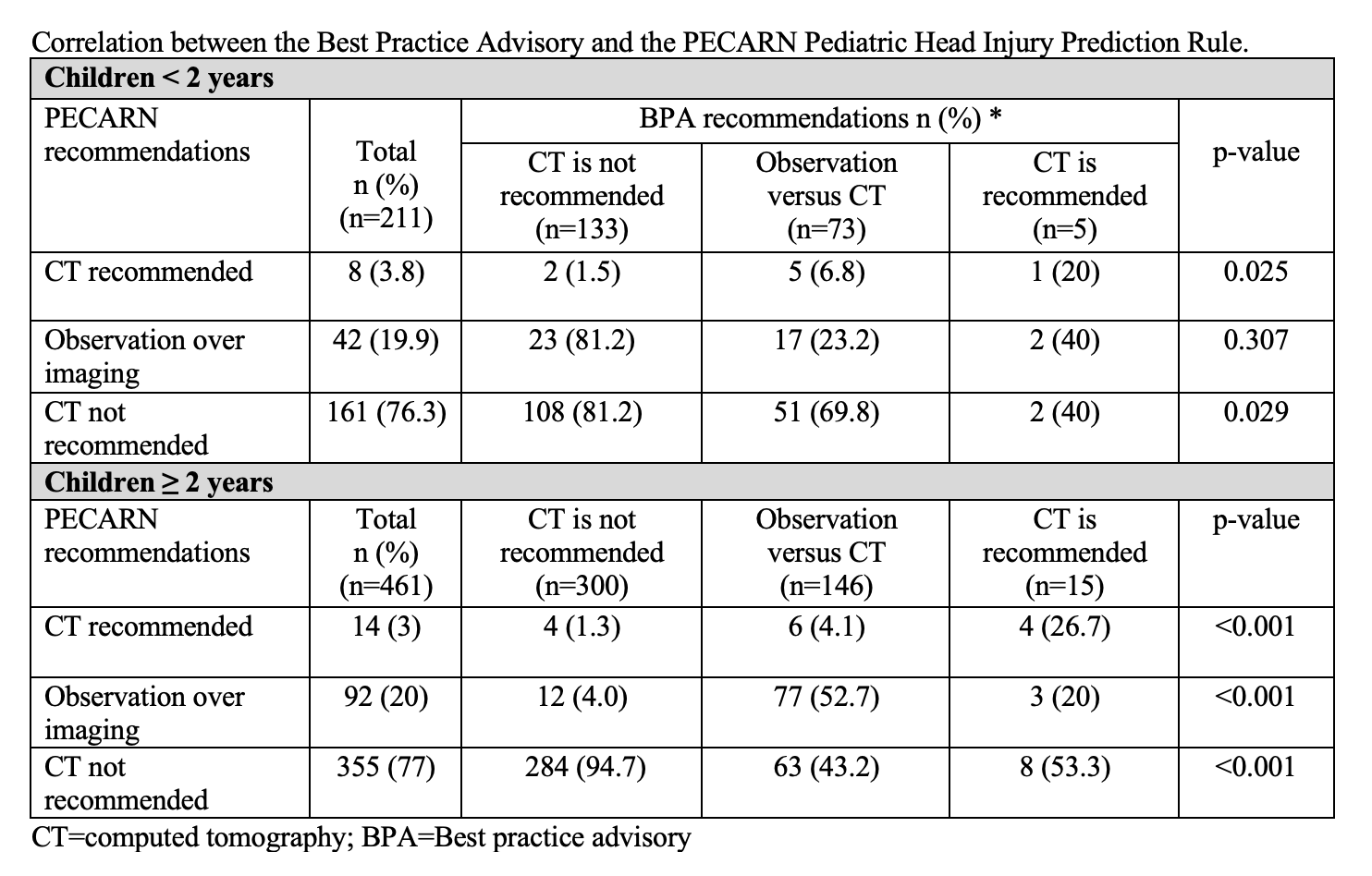
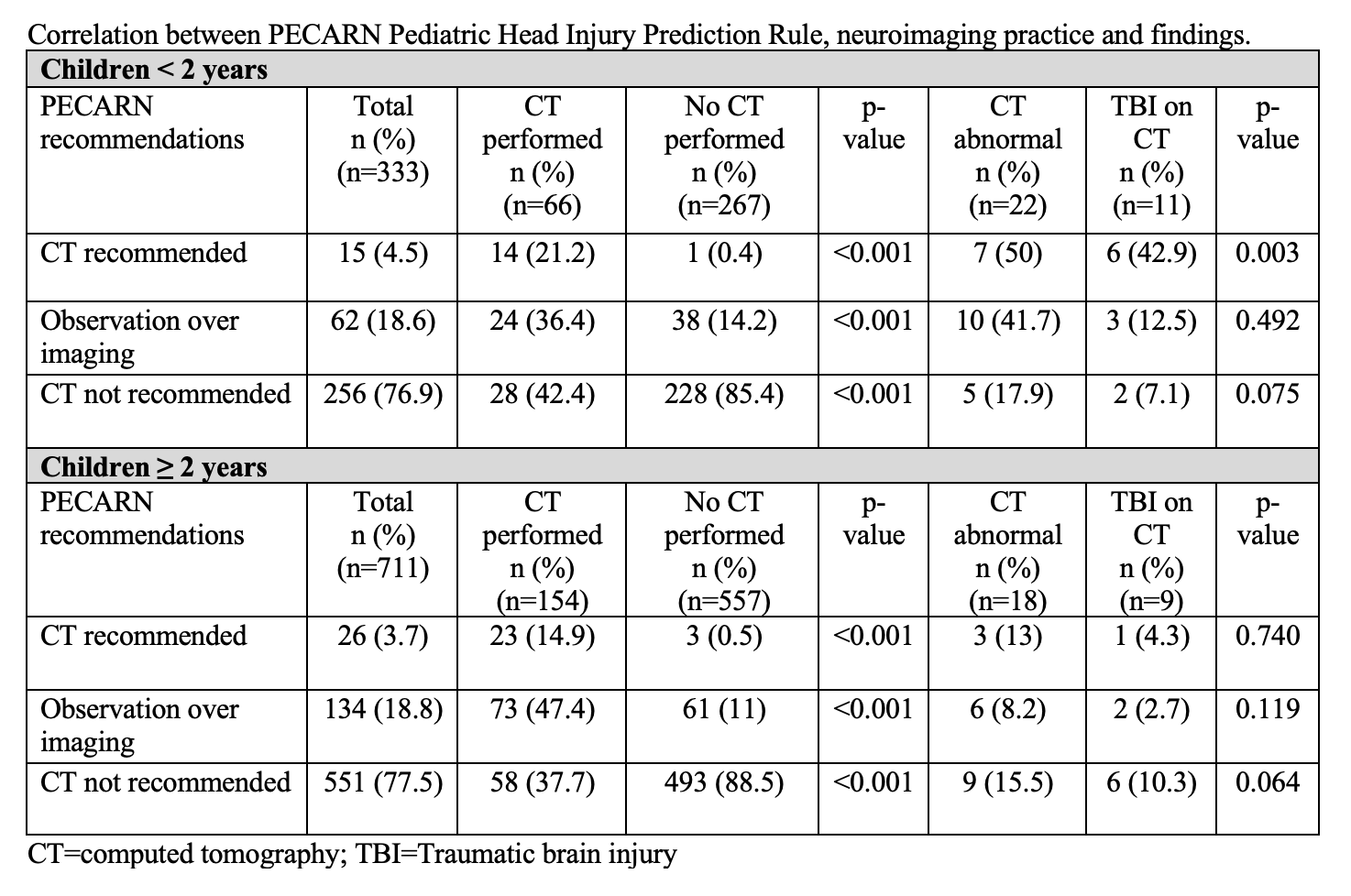
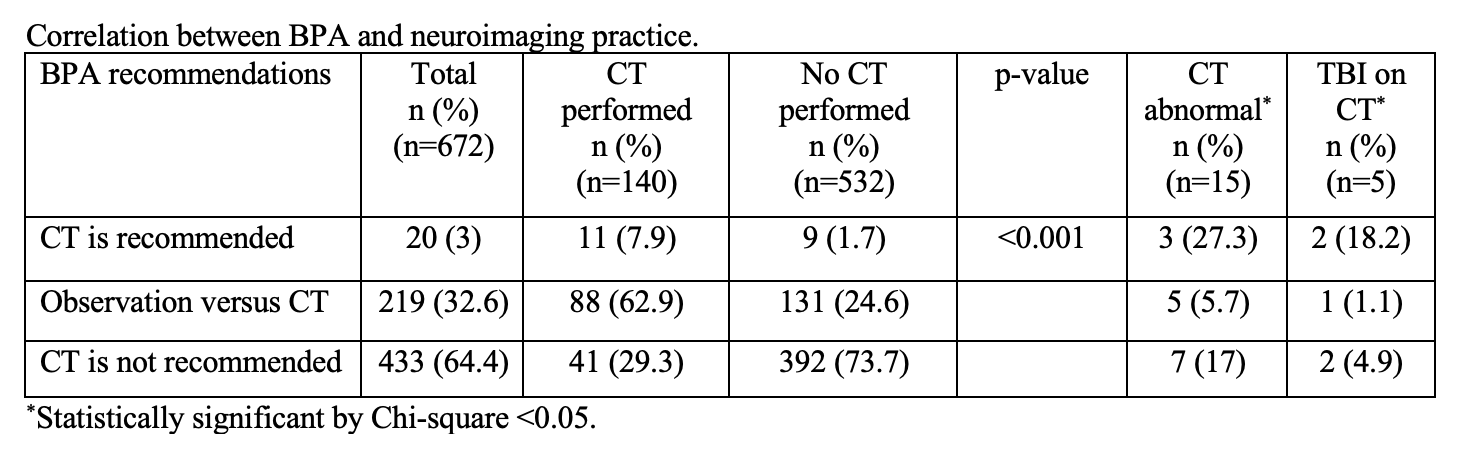
Results: We identified 1044 patients that met inclusion criteria. BPA/PECARN agreement was 73.1%, while BPA recommendation in concordance with head CT use was 88.9%. PECARN recommendation in concordance with head CT use was 89.4%. Over a third (42.4%) of children < 2 years who received a head CT had a PECARN recommendation for no head CT (p< 0.001), of which 17.9% had an abnormal head CT, with 7.1% TBI (p=0.075). About a third (37.7%) of children ≥2 years who received a head CT had a PECARN recommendation for no head CT (p< 0.001), of which 15.5% had an abnormal head CT, with 10.3% TBI (p=0.064). Agreement among BPA/PECARN and head CT use was 81.7%. Factors associated with CT use included speech changes (OR 7.9, CI 1.2-51.1), lethargy (OR 2.3, CI 1.1-4.8), altered mood/behavior (OR 2.3, CI 1.3-4.3), and gait abnormality (OR 2.2, CI 1.1-4.49), among others.
Conclusion(s): Prediction models for ordering neuroimaging in children with blunt head trauma may aid in curbing the overuse of resources, but discrepancy remains between their recommendations and subsequent neuroimaging use. Numerous symptoms and physical findings were associated with ordering a CT against PECARN recommendations; however, this clinical decision tool would have missed clinically important traumatic brain injuries if it was strictly followed.