Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 3
88 - Comparison of Hemodynamic, Gas Exchange and Side Effects of Prostaglandin E1 in Neonates with CHD vs. Pulmonary Hypertension
Publication Number: 88.425

Sonam A. Mokha, MD (she/her/hers)
Resident Physician, PGY-2
University of California Davis Children's Hospital
Sacramento, California, United States
Presenting Author(s)
Background:
Intravenous Prostaglandin E1 (IVPGE1) is commonly used to maintain ductal patency in congenital heart disease (CHD). It is increasingly being used to maintain ductal patency in persistent pulmonary hypertension of the newborn (PPHN) associated with right ventricular failure to maintain a right-to-left pop-off shunt and as a pulmonary vasodilator. While the respiratory and hemodynamic benefits of IVPGE1 in ductal-dependent CHD are well established, its effects in patients with PPHN is not known.
Objective:
To compare the effects of IVPGE1 on hemodynamics and gas exchange in neonates with CHD and PPHN.
Design/Methods:
A retrospective chart review identified all neonates (≤30d) who received IVPGE1 from 10/1/12 to 10/31/22 at UC Davis Children’s Hospital. A total of 43 patients were identified and then stratified into CHD (n=33) or PPHN (n=10) based on their indication to receive IVPGE1. Hemodynamic, gas exchange, side effects and outcome data were collected before and after initiation of PGE1 infusion. Preductal and postductal SpO2/FiO2 (S/F) ratios, Oxygen saturation index (OSI = FiO2*Mean airway pressure*100/SpO2) and vasotropic inotrope score were calculated before and 24h after IVPGE1.
Results:
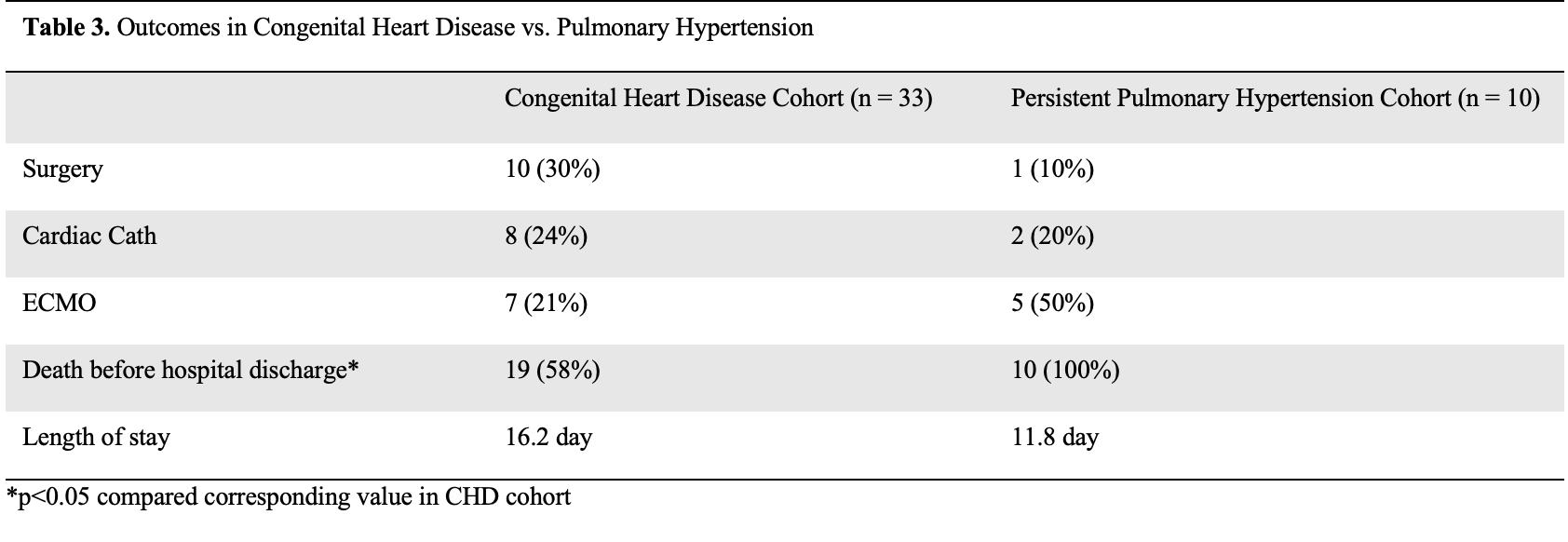
Demographic data were similar except for sex between both groups (table 1). All PPHN patients were on high frequency ventilation compared to 27% of infants in room air in the CHD group. Significant increase in oxygenation was observed in the CHD cohort after administration of IVPGE1 but not in the PPHN cohort (table 2). Vasopressor support significantly increased in PPHN and CHD groups after administration of IVPGE1. Electrolyte abnormalities and seizures following IVPGE1 were noted in both cohorts. Apneic events were noted exclusively among non-intubated patients in the CHD group. Neither cohort demonstrated any signs of gastric outlet obstruction or cortical hyperostosis. All PPHN patients died before hospital discharge (table 3).
Conclusion(s):
IVPGE1 increases oxygenation in CHD. In our institution, PPHN patients receiving IVPGE1 were sicker and IVPGE1 was associated with significant escalation of vasopressor support without any improvement in oxygenation. Careful attention to systemic hemodynamics is needed while using IVPGE1 in PPHN. Randomized trials of IVPGE1 in PPHN are warranted.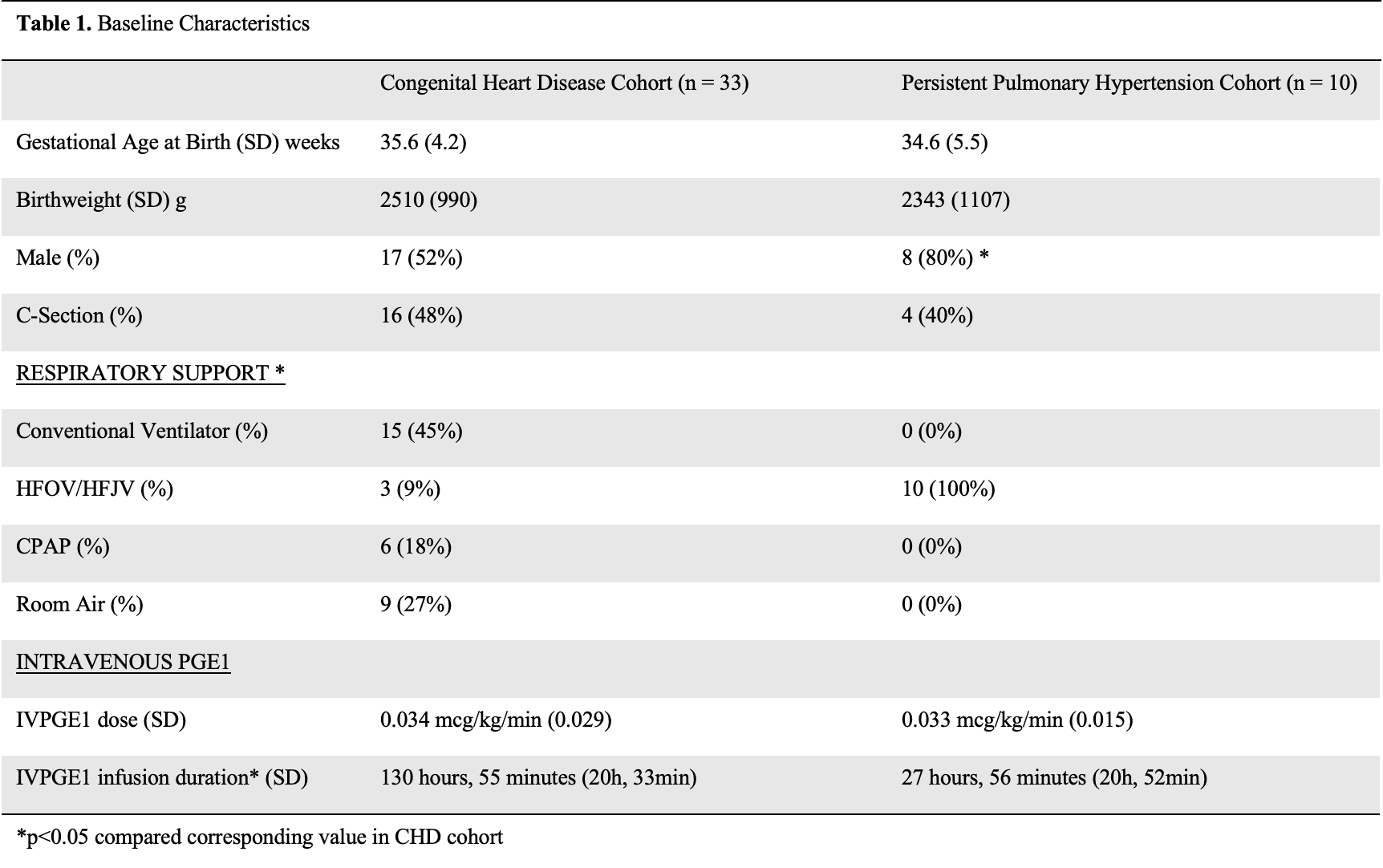
.jpg)
