Infectious Diseases
Infectious Diseases 4
424 - Patterns and Predictors of Broad-Spectrum Antibiotic Use for Community Acquired Pneumonia in Children Admitted from the Emergency Room
Publication Number: 424.418

Maheswari Ekambaram, MBBS (she/her/hers)
Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Antibiotic resistance is a pressing global concern driven by inappropriate antibiotic use. National evidence-based guidelines recommend aminopenicillins for uncomplicated community-acquired pneumonia (CAP). However, less is known about patterns and determinants of antibiotic use for CAP in the Emergency Department (ED), which can influence inpatient antibiotic choice.
Objective:
To describe antibiotic prescribing for children admitted from the ED with uncomplicated CAP and identify factors associated with broad-spectrum antibiotic use.
Design/Methods:
A retrospective cohort study of children less than 18 years old admitted from one of the 11 community and one children’s hospital ED in a single healthcare system between 2016-2021 with a diagnosis of CAP and receiving the first dose of antibiotic in the ED. We excluded children with medical complexity, severe or complicated pneumonia, intensive care unit admission, and receipt of macrolide-only antibiotics. The primary outcome was antibiotic class (narrow: ampicillin/amoxicillin or broad: all other antibiotics for pneumonia) received in the emergency room before inpatient unit admission.
Results:
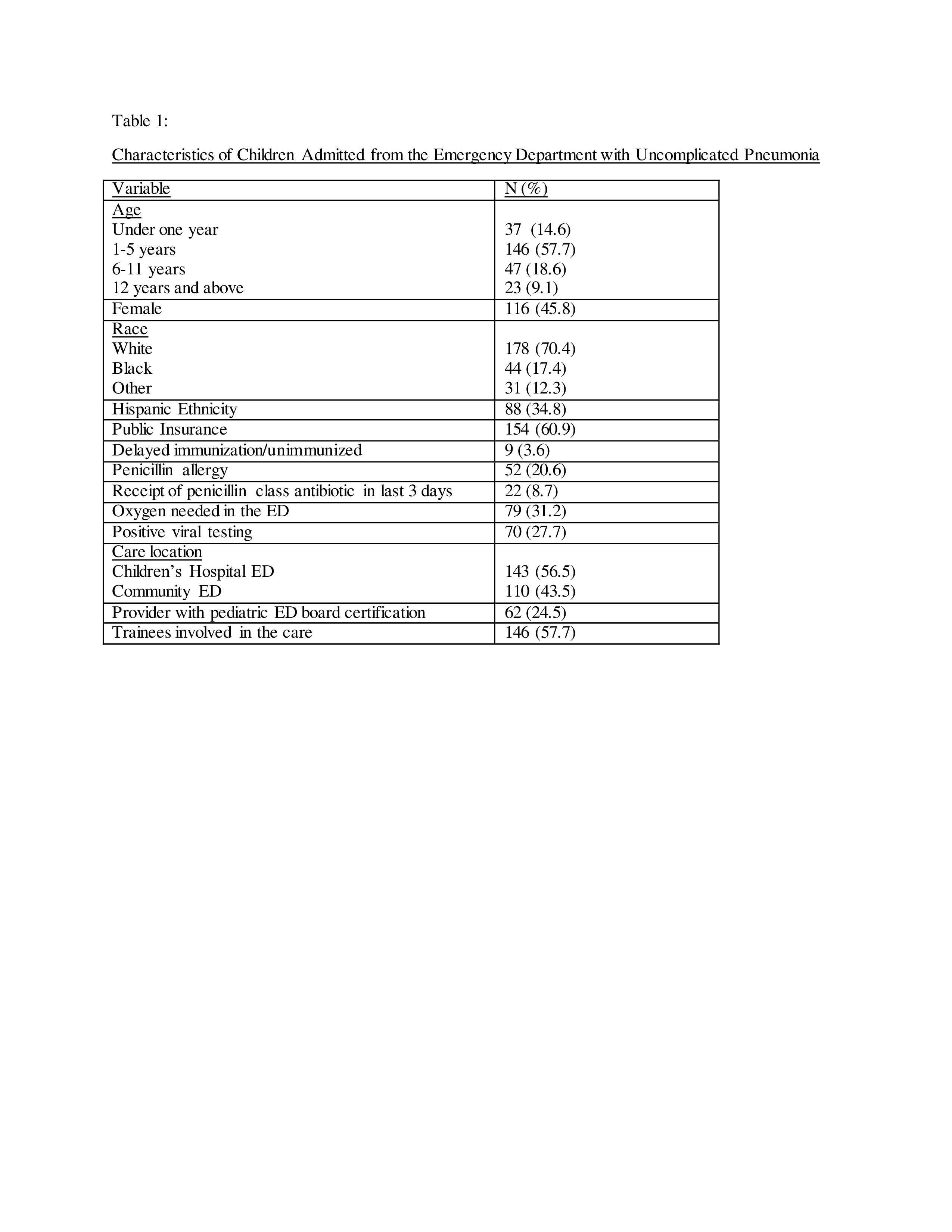
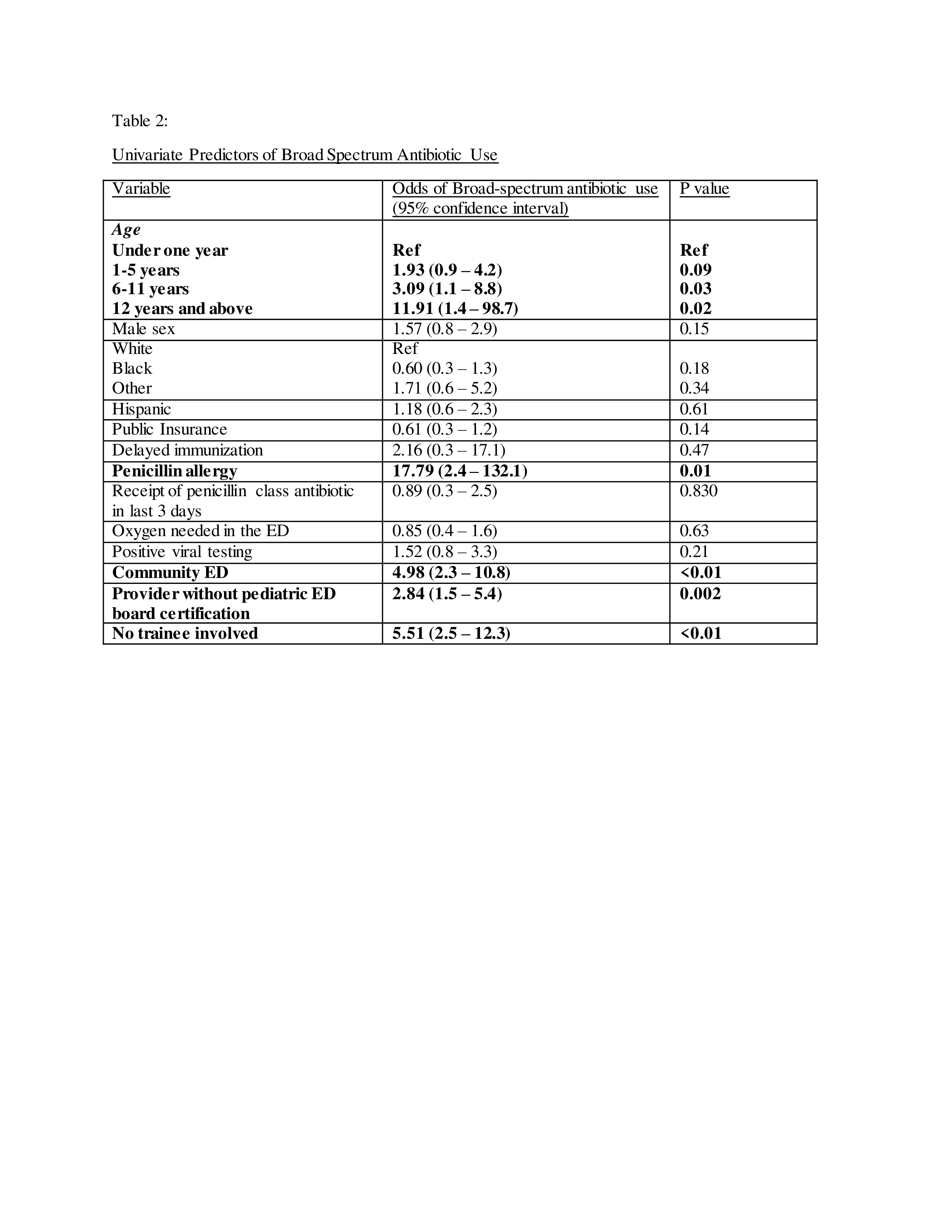
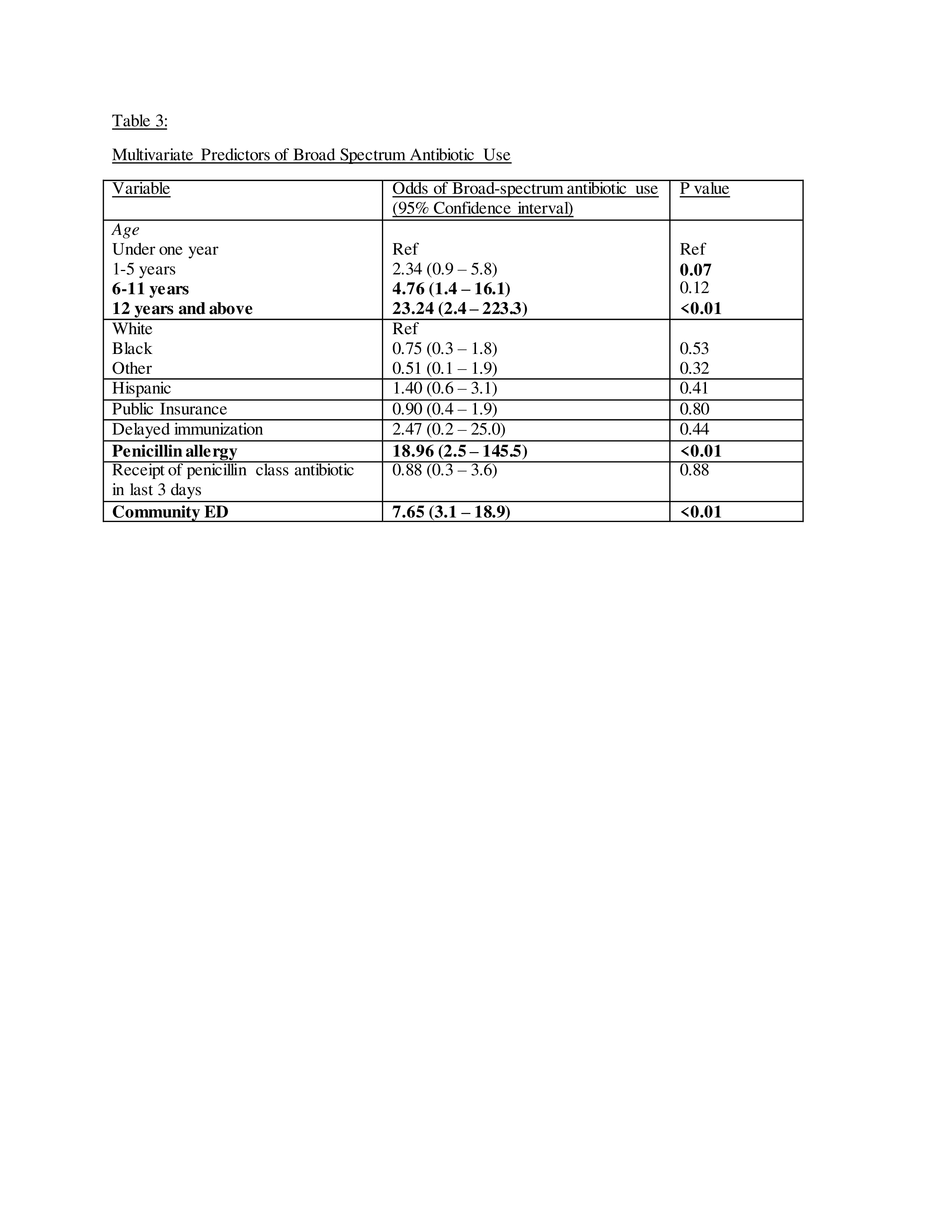
A total of 253 children were included. The majority were under five years of age (72%) and had public insurance (61%). More than half were admitted from the children’s hospital ED (56.5%) (Table 1). Broad-spectrum antibiotics were used in 79% of children, with ceftriaxone used in 70% of cases. In univariate analysis, older age, penicillin allergy, care received in a community ED, no trainee involvement, and clinician without pediatric emergency medicine board certification were associated with broad-spectrum antibiotic use (Table 2). The multivariate analysis controlled for immunization status, insurance, race, ethnicity, and receipt of penicillin-class antibiotics in the last three days before ED presentation. Care in community ED, older age, and penicillin allergy were independently associated with broad-spectrum antibiotic use (Table 3).
Conclusion(s):
The use of broad-spectrum antibiotics for uncomplicated CAP was common in the ED. Both clinical factors, such as penicillin allergy and patient’s age, and non-clinical factors, such as care in a community ED, were associated with broad-spectrum antibiotic use. These data will inform a targeted antibiotic stewardship intervention.