Medical Education: Resident
Medical Education 14: Resident 5
490 - Changing Medical Education: Firearm Violence Prevention in Pediatric & Emergency Medicine Residency Programs
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 490
Publication Number: 490.422
Publication Number: 490.422
Subah Nanda, Michigan State University College of Human Medicine, Grand Rapids, MI, United States; Amanda Schoonover, Michigan State University College of Human Medicine, Grand Rapids, MI, United States; Jasmanpreet Kaur, Michigan State University College of Human Medicine, Grands Rapids, MI, United States; Annie Vu, Michigan State University College of Human Medicine, San Jose, CA, United States; Jeff Haus, DO, Corewell Health, Grand Rapids, MI, United States; Christopher Benner, Michigan State University College of Human Medicine, Hudsonville, MI, United States

Subah Nanda, BS (she/her/hers)
Medical Student
Michigan State University College of Human Medicine
Grand Rapids, Michigan, United States
Presenting Author(s)
Background: Physicians are uniquely positioned to provide firearm safety counseling (FSC), an effective injury prevention strategy, yet few practice FSC due to limited training and other barriers. Despite this, firearm violence prevention education (FVPE) is seldom taught in graduate medical education (GME).
Objective: Our objectives were to provide FVPE to Pediatric and Emergency Medicine (EM) residents, characterize barriers to FSC, and assess the intervention’s effect on physician confidence, comfort, and perceived barriers.
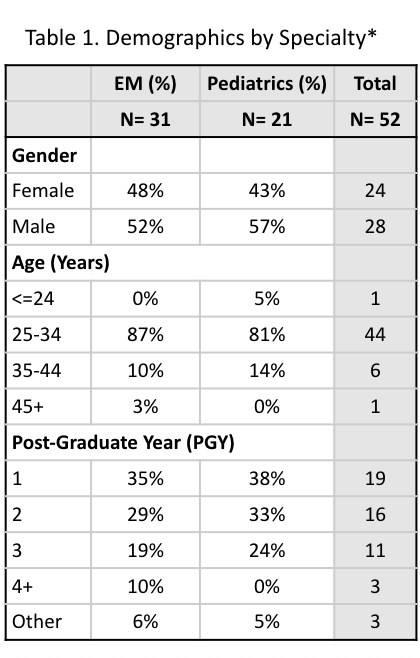
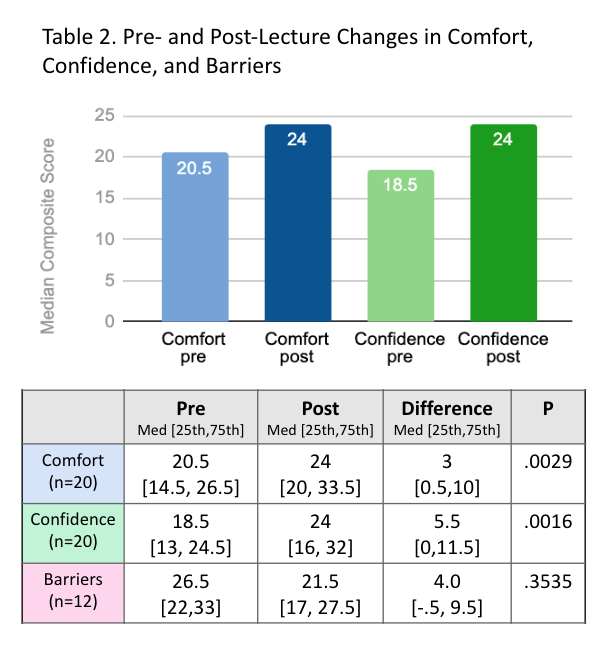
Design/Methods: We recruited a cohort of EM and Pediatric residents from an urban academic medical center. The FVPE intervention was a pre-recorded lecture with a question and answer session. Pre and post surveys collected data on demographics, prior firearm experience, and FSC. The key outcomes were changes in comfort, confidence, and barriers, which were collected in 11-point likert scale (0=not at all, 10=extremely). We calculated descriptive statistics and assessed the effect of FVPE on key outcomes. Median composite scores—a sum of items related to comfort, confidence, or barriers—were analyzed using Wilcoxon Signed-Rank test (ɑ= 0.05).
Results: 52 residents completed the pre-survey, of which 20 completed the post-survey. 90% of residents reported interest in learning about FSC. As compared to Pediatric residents, EM residents had greater prior firearm experience, including firearm use (70% vs 46%), education in GME (40% vs 20%), and treating injury (73% vs 40%). Comfort (Δ3 [10,0.5], p=0.003) and confidence (Δ5.5 [-11.5, 0], p=0.001) improved after the intervention for all, with EM residents showing greater improvement over Pediatric residents. Having “too little time” was the barrier most likely to prevent FSC for all residents. Pediatric residents were less likely to counsel due to “worry of damaging relationships” and ability to “identify those at risk”. Barriers’ impact on FSC increased post-intervention, however this change was not statistically significant (Δ4, p=0.35). These barriers were more likely to prevent Pediatric (med: 29, sd: 13) than EM residents (med: 16, sd: 14) from FSC.
Conclusion(s): FVPE improved comfort and confidence in this cohort of EM and Pediatric residents. We found differences in perceived barriers to FSC between the specialties, emphasizing both the need for FVPE in GME and highlighting ways to tailor curricula to the specific needs of medical specialties.
.png)
