Hospital Medicine: Clinical
Hospital Medicine 6
755 - Hospital Acquired Venous Thromboembolism in Floor Level Patients: A Descriptive Study
Publication Number: 755.415

Nicholas Tan, DO
Fellow
Phoenix Children's Hospital
Scottsdale, Arizona, United States
Presenting Author(s)
Background:
Venous Thromboembolisms (VTEs) are a leading cause of morbidity and mortality among hospitalized pediatric patients. Despite increasing understanding of the clinical factors contributing to VTEs among a variety of populations, patients receiving acute care have been significantly less studied. As acute care providers continue to manage patients of increasing medical complexity and technology dependence, an understanding of the clinical context of hospital acquired complications requires further investigation. This need has been heightened during the COVID-19 pandemic given the prominent role of COVID-related illnesses (Multisystem Inflammatory Syndrome in Children and pneumonia), which have been shown to increase VTE risk.
Objective:
To describe the demographic and clinical factors present in patients diagnosed with hospital-acquired VTEs receiving acute care.
Design/Methods:
A retrospective chart review was performed on patients who received acute care during admission to Phoenix Children’s Hospital from January 1, 2019 to December 31, 2021. Patients aged 0-18 years old who were diagnosed with a VTE after 48 hours of admission were included. Oncology patients were excluded. ICD-10 codes and an institutional database of patients with VTEs was utilized to identify qualifying patients. A manual chart review of demographics, admission characteristics, and associated diagnoses was completed.
Results:
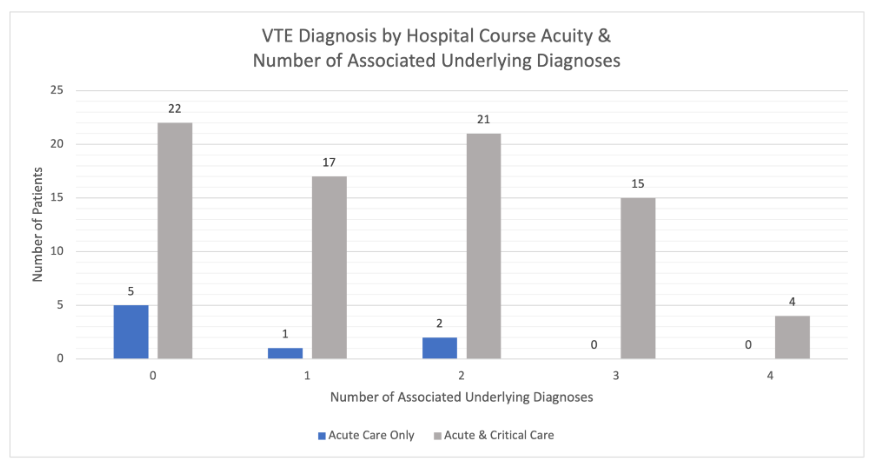
A total of 119 patients initially met inclusion for our study. After further stratifying the patients, 32 post-operative cardiology patients were excluded, with 87 patients remaining for further analysis. Eight patients (9.2%) received exclusively acute care during admission, with 79 patients (90.8%) receiving both critical and acute care. Forty-six VTEs (52.9%) were diagnosed while receiving acute care, while 41 (47.1%) occurred while receiving critical care. Sixty patients (68.9%) had one or more diagnoses of a condition associated with increased VTE risk. There were 65 catheter-associated VTEs (74.7%) and 22 non-catheter-associated VTEs (25.3%). There were no VTEs (0%) as a result of COVID-related illnesses.
Conclusion(s): Although most patients diagnosed with hospital-acquired VTEs required critical care during admission, more VTEs were diagnosed while receiving acute care. Medical conditions previously described as risk factors for VTE and indwelling catheters continue to commonly accompany hospital-acquired VTEs. COVID-related illnesses were not found in any cases, potentially reflecting vigilant management in the setting of increased awareness of VTE risk in this population.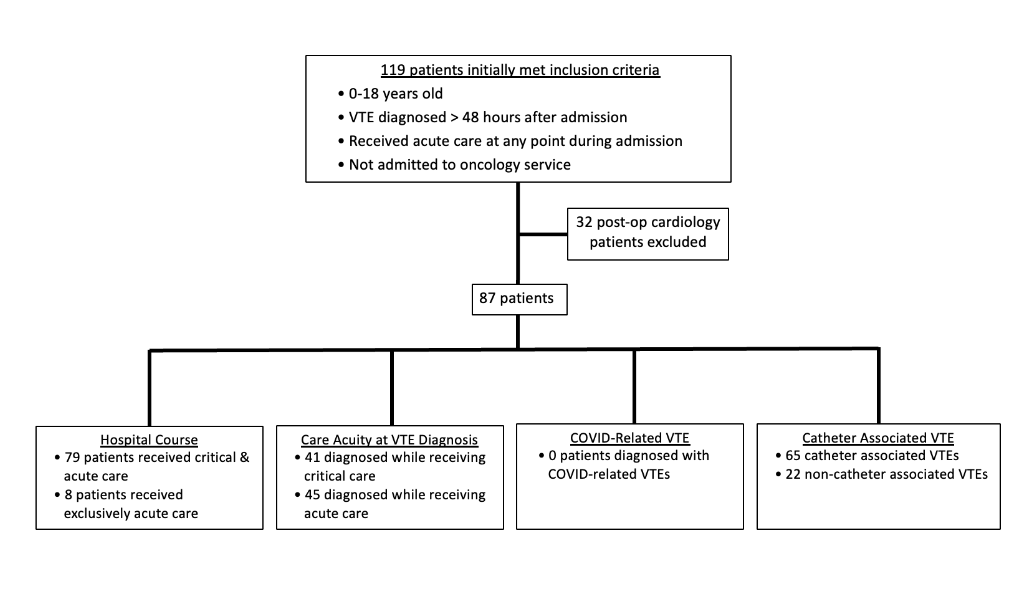
.png)