Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 6
760 - Outcomes of High-Flow Nasal Cannula Use in Patients Hospitalized with non-Severe Bronchiolitis
Publication Number: 760.415

Matthew C. Bugada (he/him/his)
Medical Student
University of Cincinnati College of Medicine
Montgomery, Ohio, United States
Presenting Author(s)
Background:
Bronchiolitis is the leading cause of hospital admission for children less than two years of age. It is primarily treated with supportive care, particularly nasal suctioning to reduce respiratory distress. High-flow nasal cannula (HFNC) has become commonplace for the treatment of hospitalized patients in pediatric intensive care units (PICU) and on inpatient floors. There has been an increase in HFNC use over the past several years, despite evidence showing no improved outcomes for patients and increased healthcare costs.
Objective: We hypothesized the use of HFNC in infants with non-severe bronchiolitis will be associated with an increased length of hospital admission, likelihood of admission to the PICU, and missed feeds.
Design/Methods: All patients admitted to Cincinnati Children’s Hospital Medical Center for non-severe bronchiolitis between December 2015 and September 2021 were eligible for inclusion. We defined non-severe bronchiolitis using measures proposed in a prior randomized controlled trial, specifically meeting all three of the following criteria: oxygen saturation of greater than 90% on < 3L of standard nasal cannula, a respiratory rate below 70 breathes per minute, and no altered mental status. The primary predictor included in our models was HFNC therapy, and we included age, sex, and insurance status as covariates. We used the appropriate regression models to assess the relationship between HFNC therapy use and three outcomes: number of missed feeds, length of hospital stay, and admission to PICU.
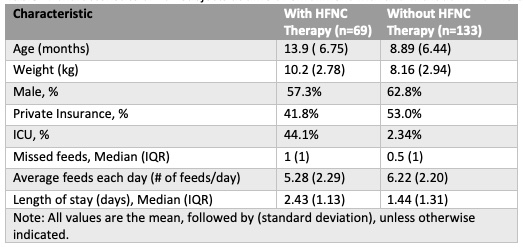
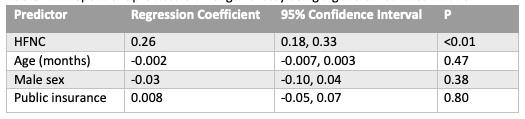
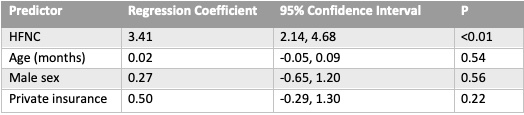
Results: There were 3190 eligible patients over our 6-year study period, and we randomly selected 202 patients for detailed chart review and abstraction. Characteristics of the cohort are included in Table 1. HFNC was found to be an independent significant predictor of length of stay in the hospital, with children who received HFNC staying longer in the hospital (Table 2;p< 0.01). The use of HFNC was also associated with an increased adjusted odd ratio of 3.41 (95% confidence interval of 2.14-4.68) for PICU admission (Table 3).
Conclusion(s): HFNC therapy in non-severe bronchiolitis was independently associated with increased risk for admission to the PICU and duration of hospital admission when controlling for the covariates of age, sex, and insurance status. No association was found between HFNC therapy and missed feeds. Limitations of the study include a small sample size as well as not controlling for additional covariates such as admitting unit, supplemental oxygen therapy, and age-matched vitals. These findings support initiatives to safely reduce the use of HFNC in non-severe bronchiolitis.