Medical Education: Resident
Medical Education 15: Resident 6
501 - A Longitudinal Program in Narrative Medicine for Trainees in Pediatrics
Publication Number: 501.422

Samantha Rosenblum, MD (she/her/hers)
Resident physician
UMass Memorial Children's Medical Center
Worcester, Massachusetts, United States
Emily Greenstein, MD (she/her/hers)
Assistant Professor of Pediatrics, Pediatric Cardiology
UMass Memorial Children's Medical Center
Sudbury, Massachusetts, United States
Presenting Author(s)
First Author(s)
Background:
Research has supported the inclusion of narrative medicine in pediatrics curricula, however there remain limited examples of successful implementation. Narrative medicine will “teach residents to listen and reflect, improve humane and effective communication, promote more meaningful patient interactions, and foster resilience among pediatric residents.” This curriculum serves to support pediatrics trainees and increase professional fulfillment.
Objective:
This curriculum aims to help learners: (1) demonstrate an understanding of narrative medicine, (2) participate in reflective writing and discussion, (3) convey the impact of narrative reflection on clinical and professional performance and (4) build a safe environment for sharing.
Design/Methods:
Monthly sessions over one academic year introduce a theme and discussion questions, followed by close reading and a writing exercise.
Results:
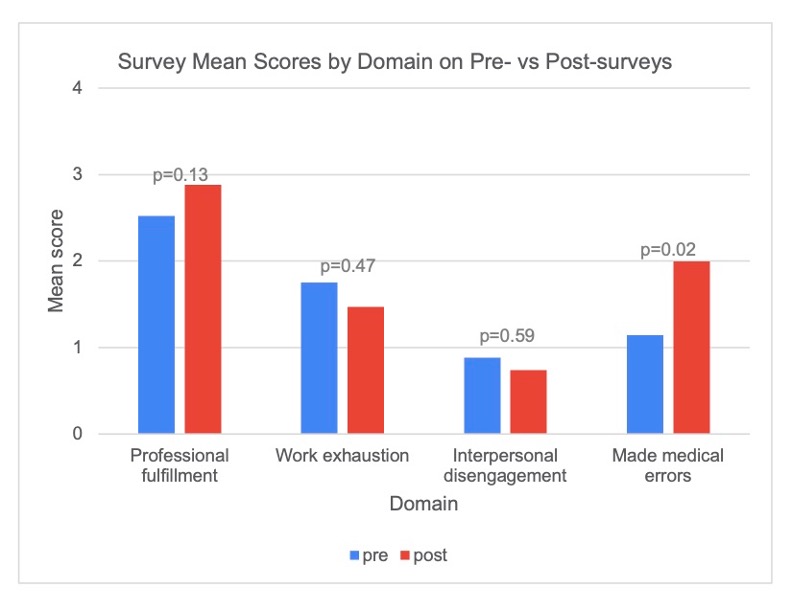
We utilized surveys that incorporate the Stanford Professional Fulfillment Index questionnaire (SPFI), which include three composite scales: professional fulfillment, work exhaustion, and interpersonal disengagement. The post-intervention survey also asked participants about their experience with sessions. Using the SPFI, we performed a two-sample t test, treating each survey as an independent sample. The analysis showed improvement on the three domains above. On the post-intervention survey, respondents all chose “very good” or “excellent” when asked about the quality of sessions, and the relevance to residency. 71% of respondents noted the importance of self-reflection. One participant wrote: “They gave me a space to express myself. They helped me find more meaning in medicine.”
Conclusion(s):
The survey responses demonstrated the value of this program. Demanding schedules placed limitations on resident involvement. We addressed this by scheduling sessions during protected didactic time. This curriculum is transferrable to other residencies. The intervention is low-cost and requires engaged faculty, access to readings and allotted didactic time. With this curriculum, other institutions can increase professional fulfillment among residents and foster a culture of reflection within their department.