Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 7
768 - Discharge Variation in Febrile Infants at a Community Hospital
Publication Number: 768.416

Mohamed M. Radwan, MD (he/him/his)
Pediatric Resident
The Children's Hospital at Monmouth Medical Center
Long Branch, New Jersey, United States
Presenting Author(s)
Background:
There is substantial difference in managing febrile infants < 60 days, mainly due to variations in infants' clinical presentation and severity of illness. In 2021, the AAP released an update to the Clinical Practice Guidelines (CPG) for evaluating and managing well-appearing febrile infants 8-60 days old, aiming to provide evidence-based, standardized care.
At our institution, we encountered some variability in initial management of febrile infants. So, we participated in a national quality improvement (QI) project to improve adherence to the new CPG in our ED and inpatient pediatric unit.
Objective:
Our objective is to identify well-appearing febrile infants (8-60 days) with hospital stay >36 hours and to explore reasons behind extended hospitalization.
Design/Methods:
We performed a retrospective chart review on infants 8-60 days of life who presented to Monmouth Medical Center Emergency Department (MMC ED) from January 1st to October 31st, 2022. We included well-appearing infants with fever ≥100.4F in the past 24 hours.
Exclusion criteria included infants who are ill-appearing, premature < 37 weeks, has chronic medical conditions, bronchiolitis, evidence of specific bacterial infection and with recent antibiotic treatment or immunization within the last 48 hours.
A subset analysis was performed on infants admitted to the inpatient unit for more than 36 hours of initial evaluation.
Results:
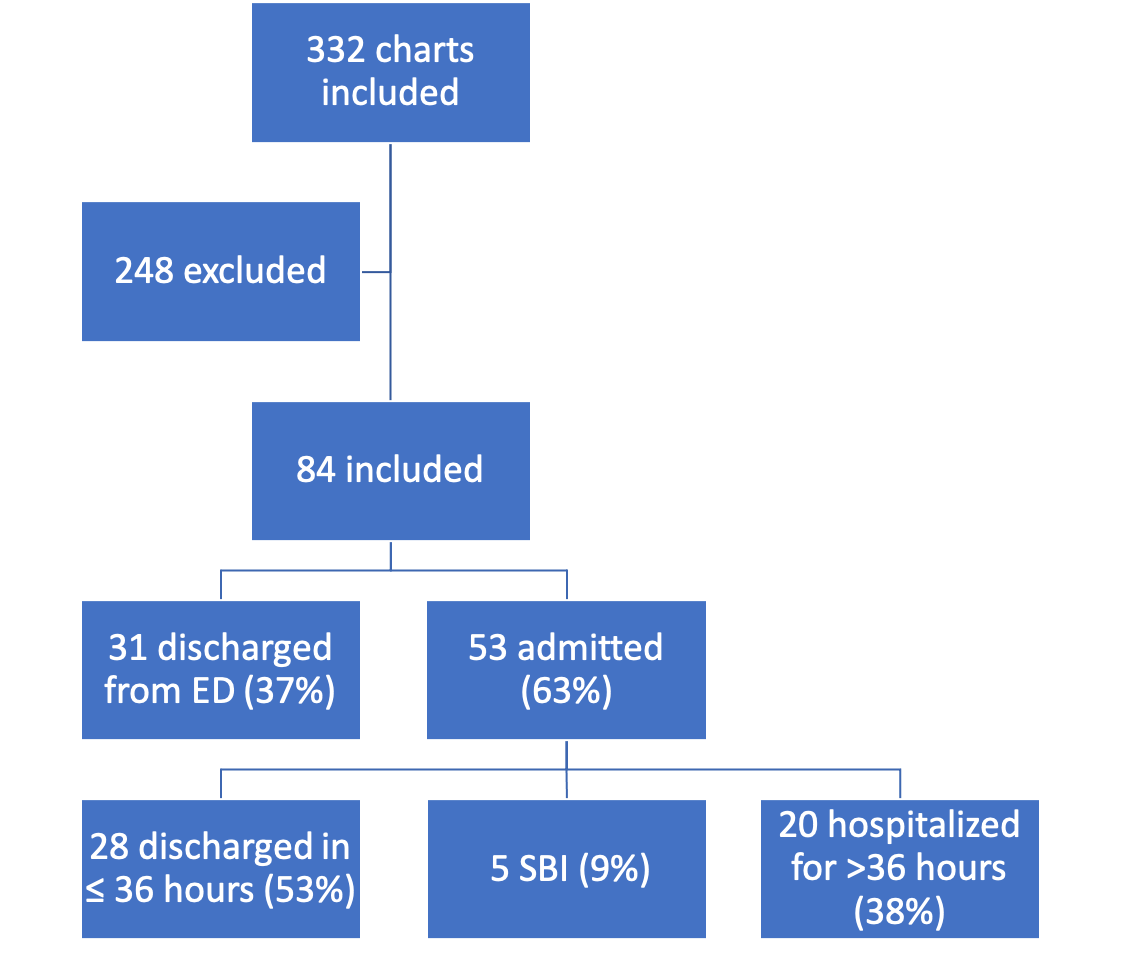
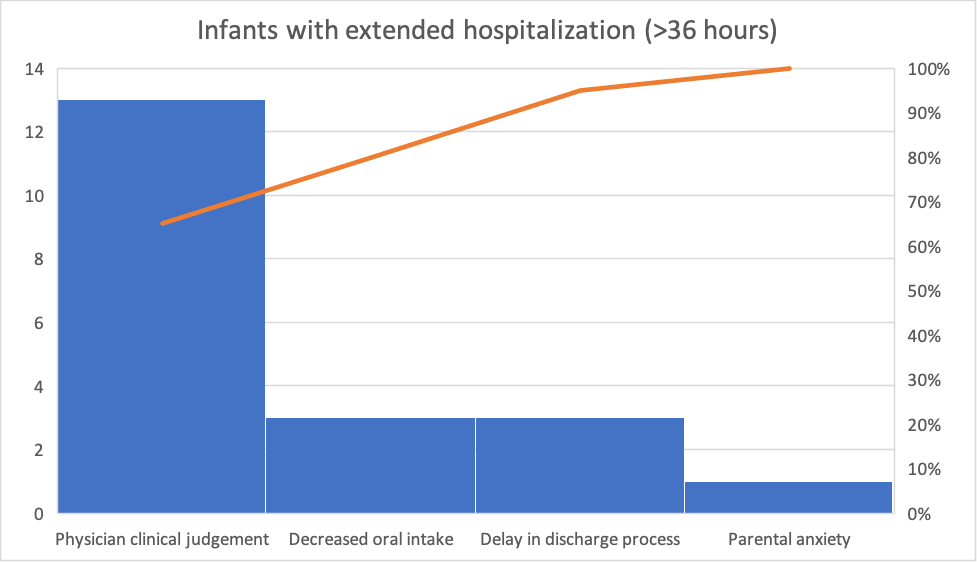
Out of 332 patients, 84 patients met the inclusion criteria (figure 1). Of these patients, 63% were hospitalized and 37% were discharged from the ED. Of the admitted patients, 9% were found to have a serious bacterial infection (SBI). Of the remaining patients, 53% were appropriately discharged in ≤ 36 hours, however, 38% of the patients were hospitalized for >36 hours despite negative culture results. A chart review was done on these patients to identify reasons behind extended hospitalization (figure 2). 65% were due to physician judgement, mainly due to progression of disease in the setting of enteroviral meningitis in 46% of patients. 15% were due to other symptoms like decreased oral intake, and the remaining 20% were due to non-clinical factors, including parental anxiety and delays in the discharge process.
Conclusion(s):
Prolonged hospitalization for well-appearing febrile infants with no evidence of SBI remains a national public health issue. Based on our data, physician judgement is the leading cause of extended hospitalization. Further research is needed to provide objective criteria in labeling the febrile infants "well-appearing" rather than excessive reliance on subjective clinical findings.