Critical Care
Critical Care 4
725 - Cryoprecipitate Use in Hospitalized Children: A PHIS Database Study
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 725
Publication Number: 725.401
Publication Number: 725.401
Kevin Doré, Weill Cornell Medicine, New York City, NY, United States; Anjile An, Weill Cornell Medicine, New York, NY, United States; Robert A. DeSimone, Weill Cornell Medicine, New York, NY, United States; Marianne Nellis, Weill Cornell Medicine, Cornell University, New York, NY, United States
- KD
Kevin Doré, MD (he/him/his)
Resident Physician
Weill Cornell Medicine
New York City, New York, United States
Presenting Author(s)
Background: Cryoprecipitate is often used to prevent and treat bleeding in the setting of surgery, trauma, liver failure, disseminated intravascular coagulopathy, and cancer. Despite its importance, little is known about the overall use and epidemiology of cryoprecipitate in pediatric populations.
Objective: To describe the prevalence and epidemiology of cryoprecipitate transfusions among hospitalized children in the United States from 2010-2019.
Design/Methods: We conducted a retrospective cohort study of hospitalized patients using data obtained from the Pediatric Health Information System (PHIS) database. Pediatric patient encounters (ages 0-18 years of age) receiving at least one cryoprecipitate transfusion from January 1, 2010, to December 31, 2019, were included. Associated data regarding demographics, diagnoses, complex chronic conditions, procedures during hospitalization, thrombosis, infection, and outcomes were extracted for eligible encounters.
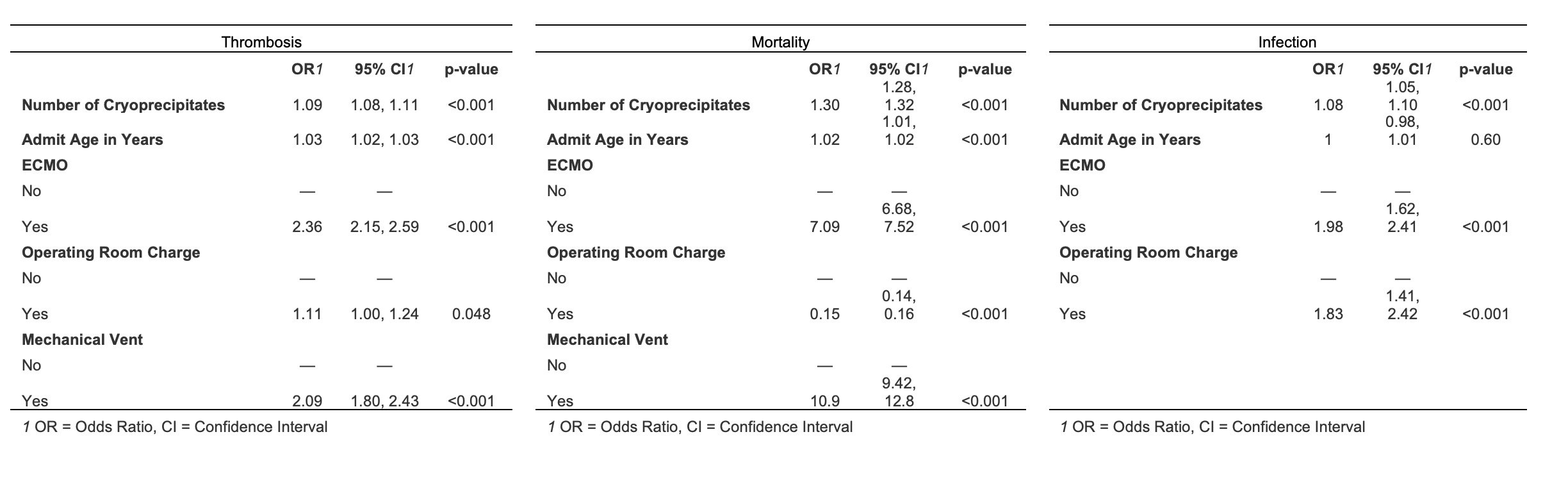
Results: There were 6,284,264 total hospital encounters from 47 hospitals within the PHIS database. Of those encounters, 76,614 children received at least one cryoprecipitate transfusion, resulting in a prevalence of 1.23% (95% CI 1.22-1.24). The proportion of hospitalizations requiring a least one cryoprecipitate transfusion was constant over the decade studied (p=0.59). Fifty-six percent of the transfused cohort was male with a mean (SD) age of 2.5 (4.7). Eighty-eight percent of transfused children had a complex chronic condition and the most common diagnoses included diseases of the circulatory system (42%) and newborn encounters (31%). After adjusting for age, ECMO support, mechanical ventilation (except for infection), and the need for surgical intervention, every additional cryoprecipitate transfusion increased the odds of thrombosis (1.09, 95% CI: 1.08, 1.11), infection (1.08, 95% CI: 1.05, 1.10), and mortality (1.30, 95% CI: 1.28, 1.32).
Conclusion(s): Despite efforts to promote more restrictive transfusion practices, the prevalence of cryoprecipitate use has remained stable in hospitalized children in the United States over the past decade. Prospective interventional trials should focus on those children undergoing cardiopulmonary bypass surgery and neonates to investigate the safety and efficacy of cryoprecipitate in children.