Critical Care
Critical Care 4
734 - Time to Tracheostomy in Pediatric Trauma Patients Undergoing Prolonged Mechanical Ventilation
Publication Number: 734.401

Kalee L. Grassia, MD, MS (she/her/hers)
Clinical Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background:
Tracheostomies can have life-altering ramifications for both patients and families and occur in < 1% of pediatric intensive care unit (PICU) admissions. While tracheostomy placement after seven or fewer days of invasive mechanical ventilation is common in adult trauma patients, the same is not true for children. However, early tracheostomy may facilitate early mobilization and rehabilitation and improve outcome.
Objective: Among patients receiving mechanical ventilation for more than 7 days, we sought to 1. Describe the timing of tracheostomy in trauma patients and the factors associated with placement 2. Identify the impact of tracheostomy on ICU and hospital length of stay in this population
Design/Methods: Study was approved by the Cincinnati Children’s Hospital Medical Center (CCHMC) IRB (Approval # 2022-0524) with a waiver of informed consent. An existing CCHMC Trauma database was queried for patients mechanically ventilated >7 days from January 1, 2011 and December 31, 2021. Demographic, clinical, and outcome comparisons were made by Wilcoxon Rank Sum Test with Dunn’s post hoc comparison using rstatix in the R statistical package. Univariate and multivariate analysis was performed using final fit. P-values of < 0.05 were considered statistically significant.
Results: Among 145 patients ventilated for more than 7 days, 9 patients (6.2%) underwent tracheostomy, and 21 (14.4%) died. Time to tracheostomy ranged from 0-33 days with the median being 21 days. Average age of patients who received tracheostomy was 12.7 years. 14.6% of non-white or Hispanic patients received a tracheostomy while 2.1% of white patients received a tracheostomy (p=0.03). ICU length of stay was a median of 15 days for patients who were extubated and 27 days for patients undergoing tracheostomy (Figure 1). Hospital LOS was 24 days for patients who were extubated and 28 days for patients undergoing tracheostomy (Figure 2).
Conclusion(s): Median time to tracheostomy was 21 days in pediatric trauma patients at CCHMC that had undergone at least 7 days of invasive mechanical ventilation. Non-white, non-Hispanic patients were more likely to receive tracheostomy, although this significance was lost with multivariate analysis. ICU but not hospital length of stay was longer for patients undergoing tracheostomy. A better understanding of decision making and indications for tracheostomy including trials of extubation is needed to improve care and progression to rehabilitation for pediatric trauma patients. 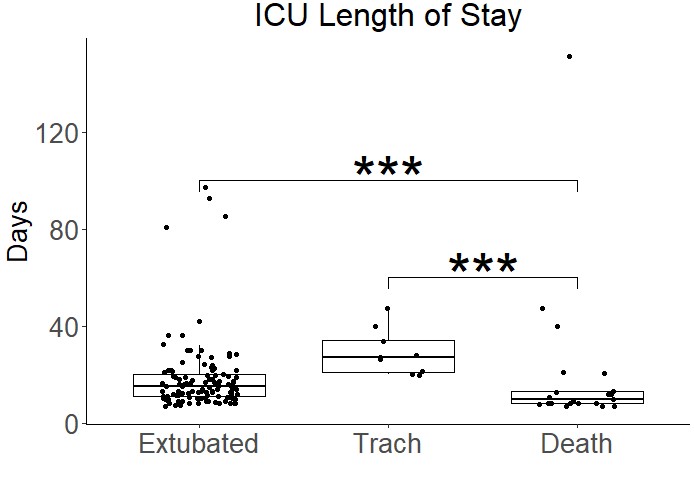
.jpg)
