Neonatal Pulmonology
Neonatal Pulmonology 6: Oxygen, Steroids
166 - Effects of Thiazides on Intermittent Hypoxemia in Extremely Preterm Infants
Publication Number: 166.438

Colm P. Travers, MD
Assistant professor
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Thiazides are frequently given to extremely preterm infants for pulmonary indications but there are limited data to guide clinical decision making.
Objective: To test the hypothesis that initiation of thiazides will be associated with fewer episodes of intermittent hypoxemia (IH) in the 14 days after initiation compared with the 14 days before initiation.
Design/Methods:
This was a single center prospective observational study including infants from 22-28 weeks’ gestation enrolled in the PreVENT study (NCT03174301). We excluded infants with missing data and infants who received furosemide during the study period. Numeric heart rate and oxygen saturation data at 1Hz were collected directly from patient monitors in the 14 days before and the 14 days after initiation of thiazides. Baseline characteristics and respiratory outcome data were collected from the electronic health record. The primary outcome was the difference in episodes of IH, defined as oxygen saturations < 85% for ≥10 seconds per hour before and after initiation of thiazides. Secondary outcomes included IH of different depths and duration, bradycardia episodes of different depths and duration, and the fraction of inspired oxygen after the initiation of thiazides. Data were analyzed by generalized linear models with repeated measures.
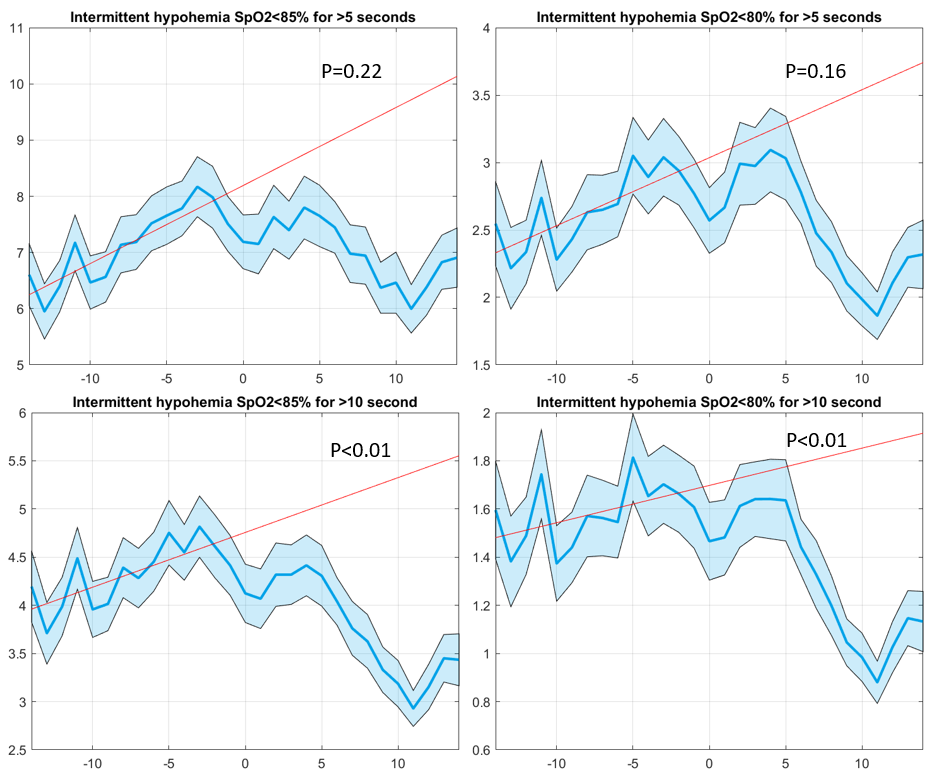
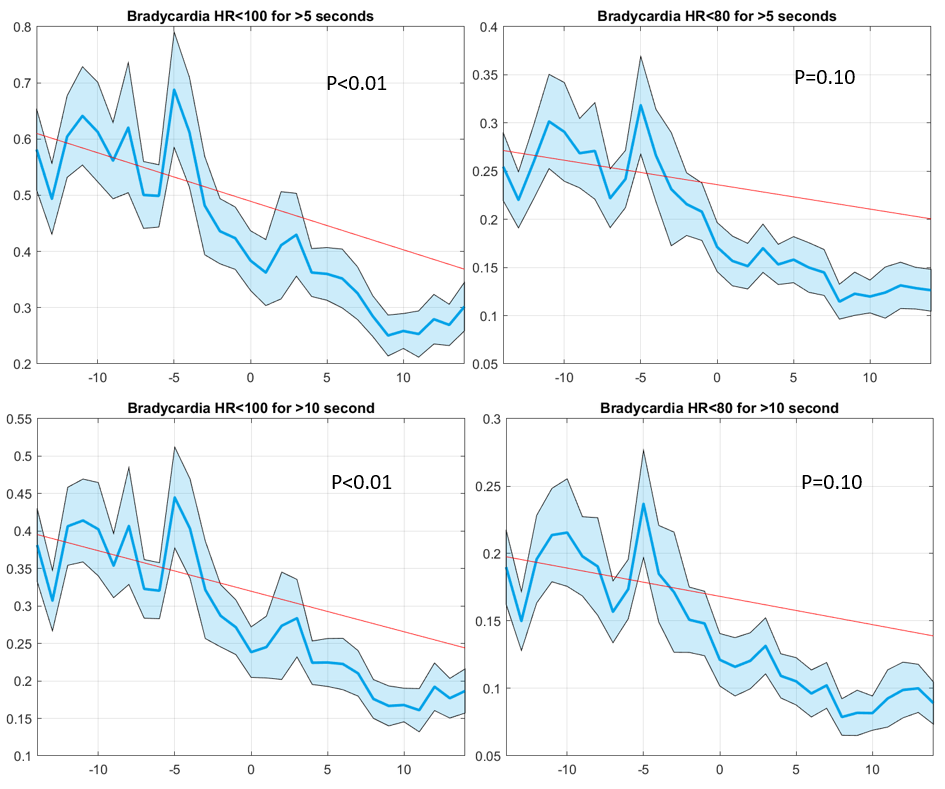
Results: There were 94 infants included with a mean (SD) gestational age of 25w 2d (12d) and a mean birth weight of 719 (185) grams. The mean age at initiation was postnatal day 35 (14). Thiazide initiation was associated with fewer episodes of IH per hour (p< 0.01). Episodes of IH < 80% for 10 seconds or longer were increased but episodes of IH lasting 5 seconds or longer did not differ [Figure 1]. Bradycardia episodes < 100 bpm decreased with exposure to thiazides but episodes < 80 bpm did not differ [Figure 2]. Regression analyses computed for the 2 weeks prior to initiation indicated that the change in episodes of IH and bradycardia were temporally related to the initiation of thiazides. The FiO2 did not differ over time.
Conclusion(s): Initiation of thiazide diuretics was associated with a decrease in episodes of intermittent hypoxemia among extremely preterm infants.