Hospital Medicine: Clinical
Hospital Medicine 6
761 - Patient Characteristics and Resource Utilization Among Hospitalized Children With Somatoform Disorder
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 761
Publication Number: 761.415
Publication Number: 761.415
Kelly Roelf, Rady Childrens hospital, San Diego, CA, United States; Manaswitha Khare, UC San Diego, San Diego, CA, United States; Tiranun Rungvivatjarus, Rady Children's Hospital/UCSD, San Diego, CA, United States; Elizabeth Mannino Avila, UCSD and Rady Children’s Hospital San Diego, San Diego, CA, United States; CHRISTIANE LENZEN, UCSD, San Diego, CA, United States; Aarti Patel, University of California, San Diego School of Medicine, San Diego, CA, United States; Erin Fisher, University of California, San Diego School of Medicine, San Diego, CA, United States; Melissa Cameron, Rady Children's Hospital San Diego, San Diego, CA, United States
- KR
Kelly Roelf, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Rady Childrens hospital
San Diego, California, United States
Presenting Author(s)
Background: Somatization is the process of experiencing one’s emotions through physical symptoms. Somatic Symptom and Related Disorders (SSRDs) are diagnosed when somatic symptoms persist and cause significant impairment. SSRDs present in 6% of hospitalized children; however, most literature characterizing SSRDs focuses on outpatient care.
Objective: To describe sociodemographic factors, clinical characteristics, and differences in management of hospitalized children with a SSRD at a tertiary children’s hospital.
Design/Methods: This retrospective, single-center study included patients 4-18 years old admitted between April 2015-December 2021 with a discharge diagnosis of a SSRD (e.g., pseudoseizure) or symptoms consistent with a diagnosis of a SSRD (e.g., sudden-onset blindness). Patients were excluded if they had an alternative diagnosis for symptoms (e.g., stroke). Clinical data were collected by chart review. Interrater reliability was performed on 9% of cases by four reviewers and discrepancies resolved by group consensus. Descriptive statistics were calculated with SPSS.
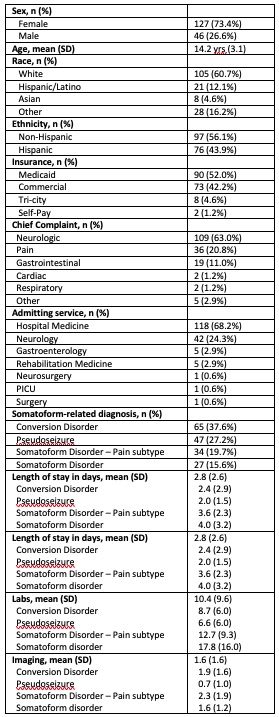
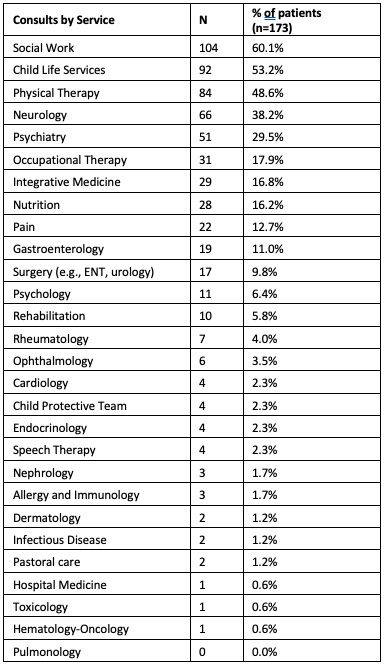
Results: Of 173 qualifying patients, the majority were female (73%), white (61%), and had Medicaid insurance (52%) (Table 1). Males were younger than females (median 13.3 vs. 14.5 yrs, p=0.009), but equally distributed across diagnostic groups. Pediatric hospital medicine admitted the majority (68%) of patients, followed by neurology (24%). The most common presenting symptom categories were neurologic and pain. Conversion disorder (CD) was the most common diagnosis, followed by pseudoseizure (PS), somatoform disorder-pain subtype (SD-P), and somatoform disorder (SD). Most patients had five or more lab studies (75.1%) and one imaging study (68.8%). Nearly all patients had one therapeutic consultation (93.6%), most often social work (57.8%) and child life (51.1%) (Table 2). Hospitalized children with PS had the shortest mean LOS (2.0 days) and, on average, the fewest labs (6.6), imaging studies (0.7), and consults (2.5). Average number of consultations (4.8) and imaging studies (2.3) were noted to be higher for SD-P, while labs were more frequently ordered for SD (17.8).
Conclusion(s): Our study found lowest resource utilization in PS compared to CD, SD-P, or SD, which often differs in initial presenting symptoms compared to the other diagnoses. Sociodemographic factors were similar across groups, suggesting these are not associated with testing considerations. More studies are needed to identify reasons for variation in resource utilization and treatment.