Public Health & Prevention
Public Health & Prevention 3
333 - Family Experiences with a 12-month Produce Prescription Program, a Mixed-Methods Analysis
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 333
Publication Number: 333.447
Publication Number: 333.447
Graciela Caraballo, George Washington University School of Medicine and Health Sciences, Washington, DC, United States; Anar Parmar, Georgetown University School of Medicine, Washington, DC, United States; Hemen Muleta, Children's National Health System, Washington, DC, United States; Noah Kim, Children's National Health System, Potomac, MD, United States; Laura Fischer, Children's National Health System, Washington, DC, United States; Kofi Essel, Children's National Health System, Washington, DC, United States

Graciela Caraballo, BA (she/her/hers)
Medical Student
George Washington University School of Medicine and Health Sciences
Washington, District of Columbia, United States
Presenting Author(s)
Background: 12.8% of households with children experienced food insecurity (FI) in 2021. There is evidence that Produce Prescription Programs (PPPs) are a viable intervention to address FI and improve diet quality in adults, however, few studies have explored the impact of PPPs in pediatric populations.
Objective: To explore the feasibility and impact of a novel PPP in a population of families with children 0-5yo who are at risk of FI and diet-related chronic diseases.
Design/Methods: To evaluate program feasibility and impact we conducted a mixed-methods study in 15 adult caregivers who completed a 12-month PPP in Washington, DC. Eligible participants had a child aged 0-5 who screened positive for FI and diet-related chronic disease risk. Individual semi-structured interviews were conducted after completion of the PPP. Interviews were recorded, transcribed, and analyzed using thematic analysis to identify emergent themes. Pre-post self-report surveys included questions derived from standardized measures of FI, nutrition, and the home food environment. Univariate descriptive statistics were used to describe demographics and survey results. Student’s paired t-test and chi-square were used to examine pre-post differences in continuous and categorical variables. Repeated measures linear regression was used to evaluate the impact of home food environment on nutrition.
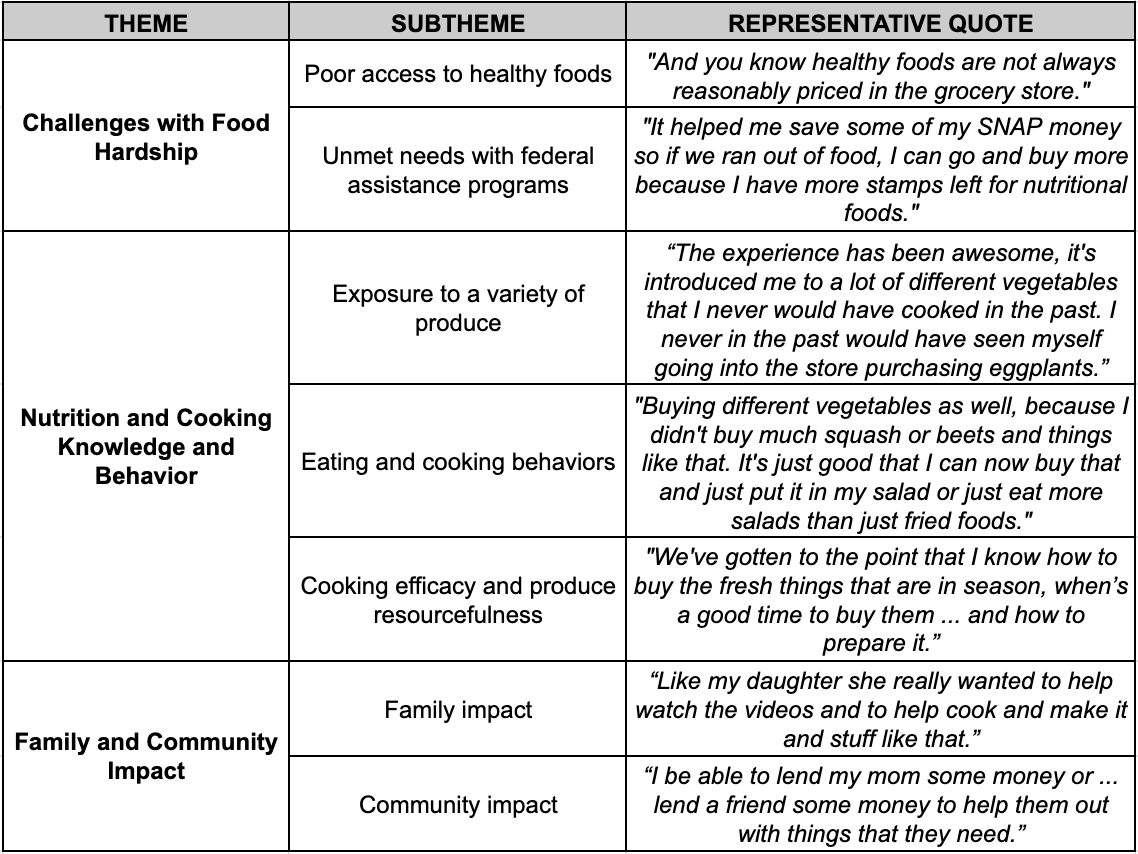
Results: Qualitative interview data were clustered into 3 themes: 1) Challenges with Food Hardship, 2) Nutrition Cooking Knowledge and Behavior, 3) Family and Community Impact (Table 1). Survey results revealed a significant decrease in individuals categorized as having “very high” FI (7% vs 43%, p=0.03). The average parent-reported daily intake of child fruit and vegetables and adult fruit and vegetable intake was higher post-intervention vs baseline (child 2.16+/-0.69 cup equivalents vs. 1.31+/- 0.67, p=0.02; adult 3.5+/-1.5 vs. 2.1+/-1.6, p=0.01). Although pre-post home food environment scores did not differ, regression models showed there was a significant independent effect of the home food environment score on child fruit and vegetable intake (F=7.1, p=0.03), indicating a more favorable home environment was associated with higher child fruit and vegetable intake.
Conclusion(s): PPPs have the potential to improve food security severity, healthy eating, and financial flexibility among families with young children who are at risk of FI. Future research should examine the sustained impact of such programs on behavioral and health outcomes among caregivers and their children.