Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 5
451 - Impact of SARS-CoV2 vaccination status and the social determinants of health of the pregnant women on the outcome of SARS-CoV2 infection in them and their newborn children
Publication Number: 451.431

Ashley Gerjets, DO
Neonatal Fellow
University of Mississippi Medical Center
Flowood, Mississippi, United States
Presenting Author(s)
Background:
The SARS-CoV2 pandemic has had a significant impact on the medical community since it began. When looking at rates of admission to ICUs, mechanical ventilation, morbidity and mortality, the severity of SARS-CoV2 infection has been found to be greater in pregnant women compared to nonpregnant women. A review of 51 cases of SARS-CoV2 infection in pregnant women reported an increase in medically indicated preterm birth and C-section delivery. In this study, 96% of deliveries occurred by C-section with a median gestational age of 36.5 weeks with delivery indications reported as SARS-CoV2 pneumonia, PPROM, and fetal distress.
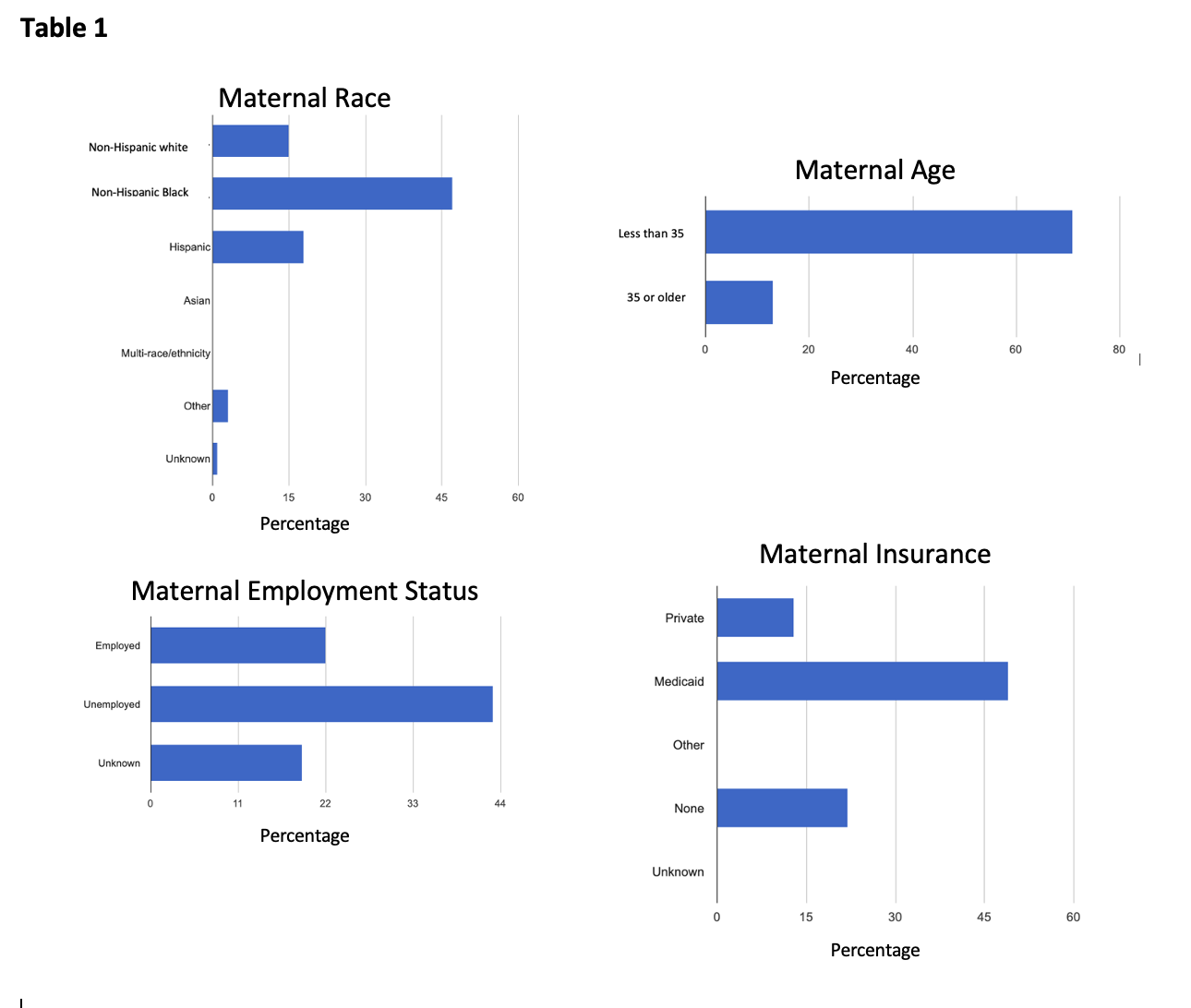
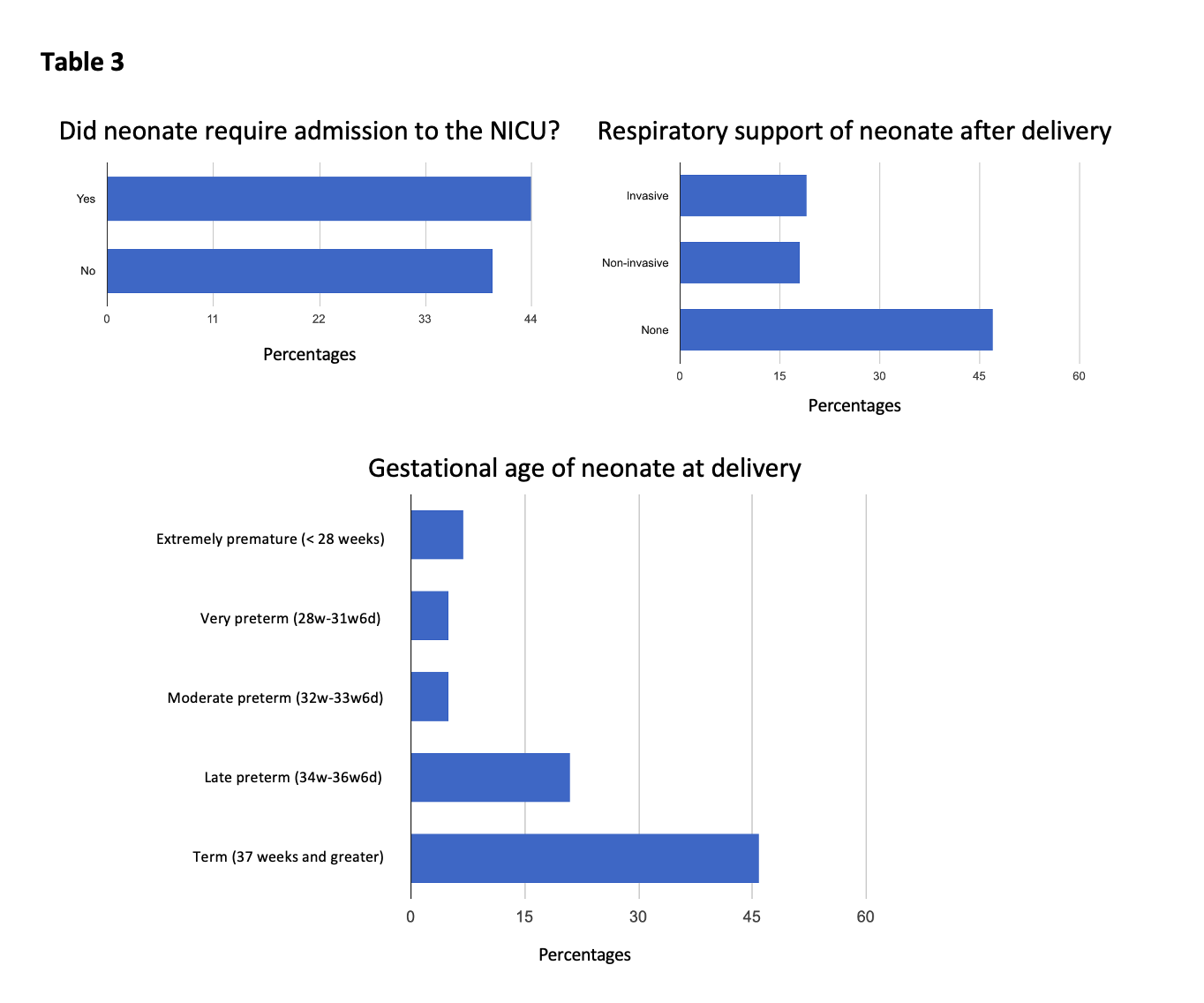
The non-white population, despite being a racial/ethnic minority of the US population, has been disproportionately impacted by infection, severe disease manifestations, and death due to SARS-CoV2. This is particularly true for Hispanic and non-Hispanic Black pregnant women. Health disparities highlighted by the SARS-CoV2 pandemic must be addressed when caring for mothers and their newborn infants. There is a need to understand how bias in the healthcare system impacts neonatal and perinatal outcomes during the SARS-CoV2 pandemic. As shown in table 1, there is a significant impact of social determinants of maternal health on the outcome of neonatal health. As shown in table 3, 54.2% of neonates required admission to the NICU. 22.6% of neonates required invasive respiratory support, 21.4% required non-invasive, and 56% required no respiratory support. 54.8 of neonates were born term with remaining born preterm.
Objective: To study the impact of SARS-CoV2 vaccination status of the pregnant women and the role of social determinants of health on the outcome of SARS-CoV2 infection in them and their newborn children.
Design/Methods: Retrospective cohort observational study based off chart review performed on SARS-CoV-2 infected pregnant women and their newborn infants, delivered at University of Mississippi Medical Center (UMMC) or transferred to UMMC from 1 March 2020 to 30 November 2021.
Results:
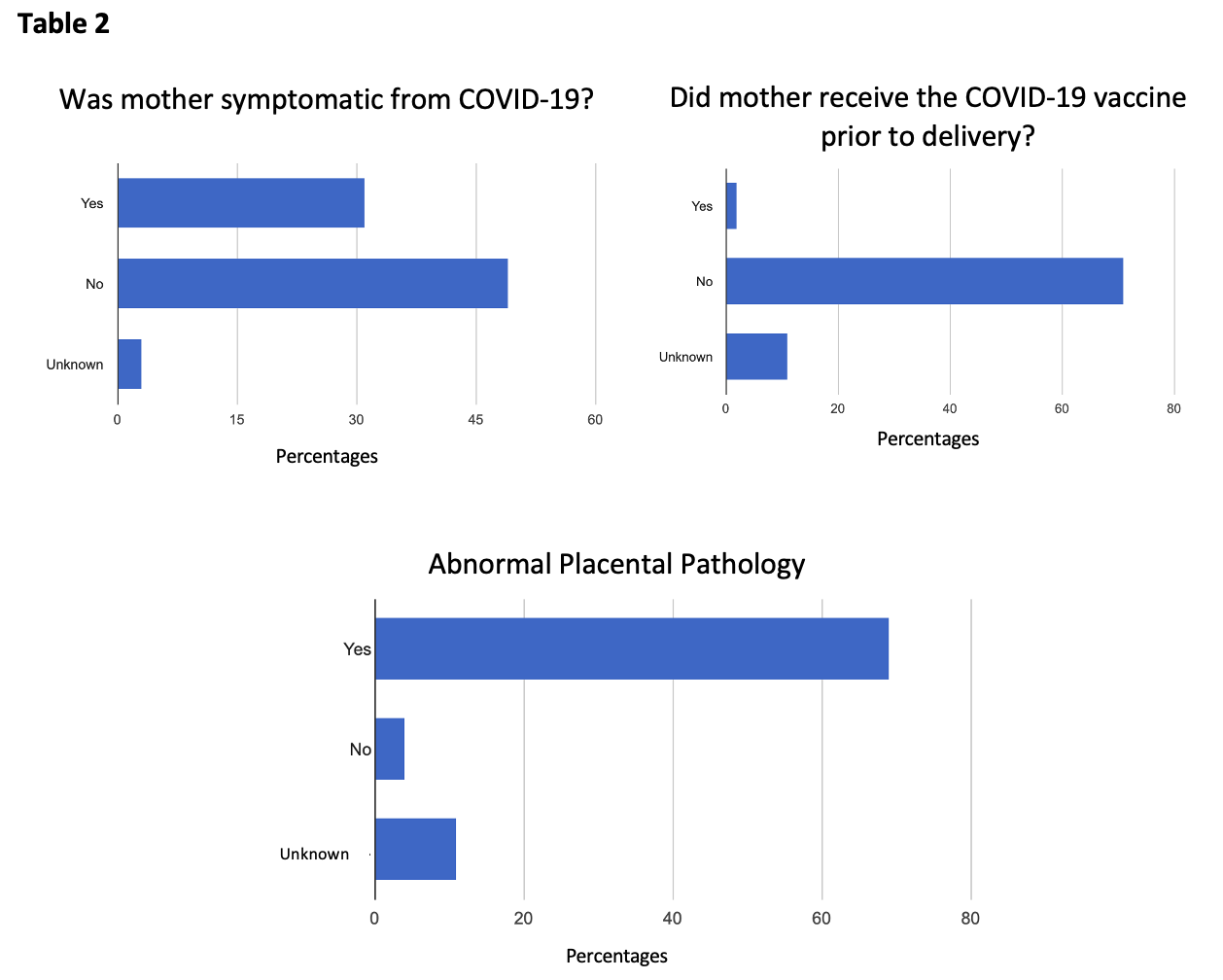
As shown in table 2, this study shows that majority of the COVID positive mothers were unvaccinated. Most of the COVID positive mothers had abnormal placental pathology including villous congestion and laminar necrosis. 36.9% of mothers were symptomatic, compared to 58.3% who were asymptomatic. 3.6% were unknown.
Conclusion(s): Our study was inconclusive about the impact of maternal COVID-19 vaccination status on the clinical outcome of their neonates due to the small number of vaccinated mothers; however, social determinants of maternal health have a significant impact on neonatal outcomes.