Emergency Medicine: All Areas
Emergency Medicine 14
378 - Emergency department facial laceration repair: Utilization of procedural sedation during repair by emergency medicine providers vs. plastic surgery consultants
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 378
Publication Number: 378.405
Publication Number: 378.405
Isabella G. Steidley, Brown University, Scottsdale, AZ, United States; David Mills, Boston Children's Hospital, Boston, MA, United States; Eric Fleegler, Boston Children's Hospital, Needham, MA, United States; Elizabeth M. Waltman, UMass Chan Medical School, Milton, MA, United States; Todd W. Lyons, Boston Children's Hospital, Wayland, MA, United States; Andrew F. Miller, Boston Children's Hospital, Boston, MA, United States; Amanda Stewart, Boston Children's Hospital, Boston, MA, United States; Michael Monuteaux, Boston Children's Hospital, Boston, MA, United States; Chris A. Rees, Emory University School of Medicine, ATLANTA, GA, United States; Assaf Landschaft, Boston Children's Hospital, Bergisch Gladbach, Nordrhein-Westfalen, Germany; Amir Kimia, Boston Children's Hospital, Boston, MA, United States

Isabella G. Steidley (she/her/hers)
Student Research Assistant
Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background: Emergency department (ED) repair of facial lacerations may require anxiolysis or procedural sedation, especially in younger children. When plastic surgery consults are obtained, there is a pre-procedural discussion between plastics and pediatric emergency medicine (PEM) providers regarding preference for sedation. This is partly due to different levels of complexity of lacerations repaired by plastic surgery versus PEM providers and, in part, by personal preference of the proceduralist.
Objective: To assess the prevalence of ED-procedural sedation use for facial lacerations with and without plastic surgery consult.
Design/Methods: Cross-sectional chart review performed at a tertiary care ED between 2016-2020. We reviewed notes of all patients with a facial laceration repaired in the ED, including pre-arrival notes, ED provider notes, plastic surgery consult notes, and follow-up notes. We excluded patients repaired with adhesive glue, steri-strips or staples and repairs performed in the operating
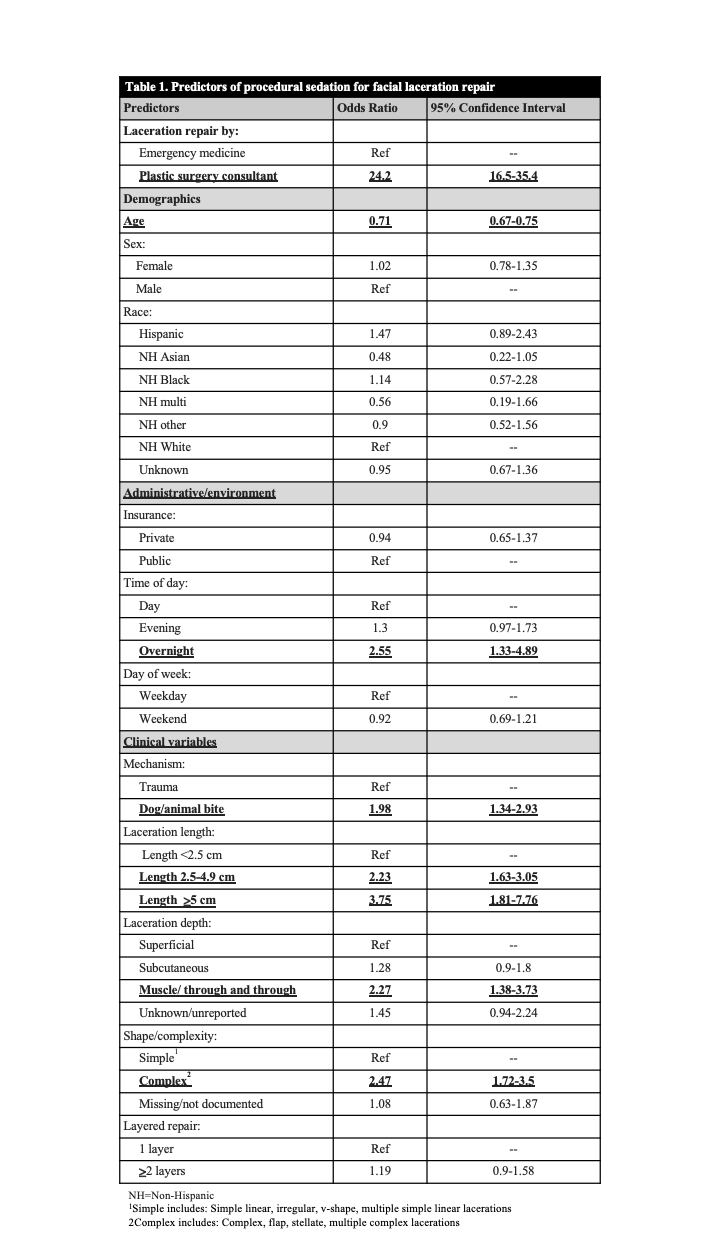
room. Procedural sedation was defined as use of ketamine, propofol+-ketamine or fentanyl, or midazolam/fentanyl during the laceration repair. Data was abstracted via natural language processing-assisted manual review. We estimated a multivariable logistic regression model with procedural sedation as the dependent variable and plastic surgery consult as the independent variable, controlled for age, sex, race and ethnicity, insurance status, day of week and time of day, laceration characteristics (length, depth, complexity) and mechanism of injury, with robust standard errors clustered on patient.
Results: During the study period, there were 4918 patient visits that met inclusion criteria. 1045/4918 (21.3%) were repaired by plastic surgery and 3873 by PEM teams. In the plastics arm, 309/1045 (29.6%) received procedural sedation compared with 64/3898 (1.6%) in the PEM group giving an aOR 24.2 (95%CI 16.5-35.4). Table 1 presents the data adjusted for demographic and clinical variables.
Conclusion(s): There is significantly higher use of procedural sedation by plastic surgery disciplines compared to PEM providers for facial laceration repairs. This is likely secondary to complexity of laceration repair, practice style/training, and expectations of providers around tolerating patient mobility during procedure. While some elements were not adjusted for (appearance, anxiety), the differences are probably substantial; thus, establishing a cohesive approach to procedural sedation for facial laceration will lead to a more uniform and safe practice.