Cardiology
Cardiology 3
709 - 3D Printed Cardiac Models for Fetal Counseling: A Novel Approach to Improve Communication
Publication Number: 709.4

Nicole T. Marella, MD (she/her/hers)
Advanced Imaging Fellow
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Most complex congenital heart disease (CHD) is now being diagnosed prenatally and the expectant parents first learn about the CHD during a fetal cardiology consultation. Current standard of care uses drawings to explain the cardiac anatomy which can result in inherent variation in how the CHD is conveyed. We propose that three-dimensional printed (3DP) cardiac models can facilitate a more uniform and concrete way to demonstrate CHD.
Objective:
Our primary aim was to demonstrate that incorporating 3DP models into fetal counseling sessions is feasible. Second, we aimed to evaluate the impact on parental knowledge, understanding, and anxiety.
Design/Methods:
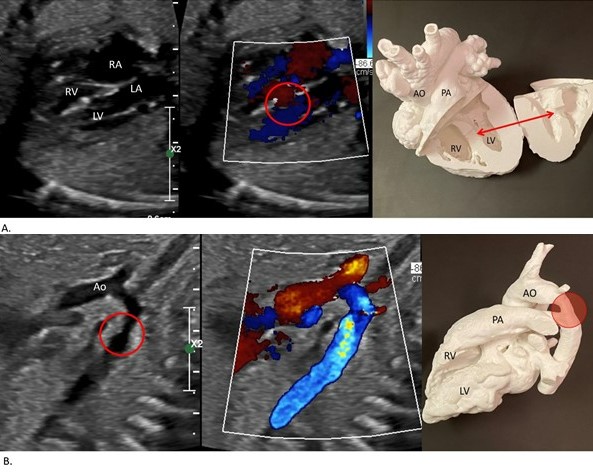
Parents with a new prenatal diagnosis of a ventricular septal defect and/or coarctation of aorta requiring counseling were approached. Providers were randomized into a Model or Drawing Group and crossed over to the other group halfway. Parents in the Drawing group were counseled with only a 2D drawing while the Model group was counseled using a 2D drawing and a 3DP model (Figure 1). Parents were asked to complete a survey after the consultation which included sections evaluating knowledge of the congenital heart lesion and expectant surgical management, self-rated understanding and attitude towards the visualization tool, and parental anxiety. An additional survey was administered to providers who conducted counseling using the Model. Outcomes between groups were assessed using Kruskal-Wallis tests.
Results:
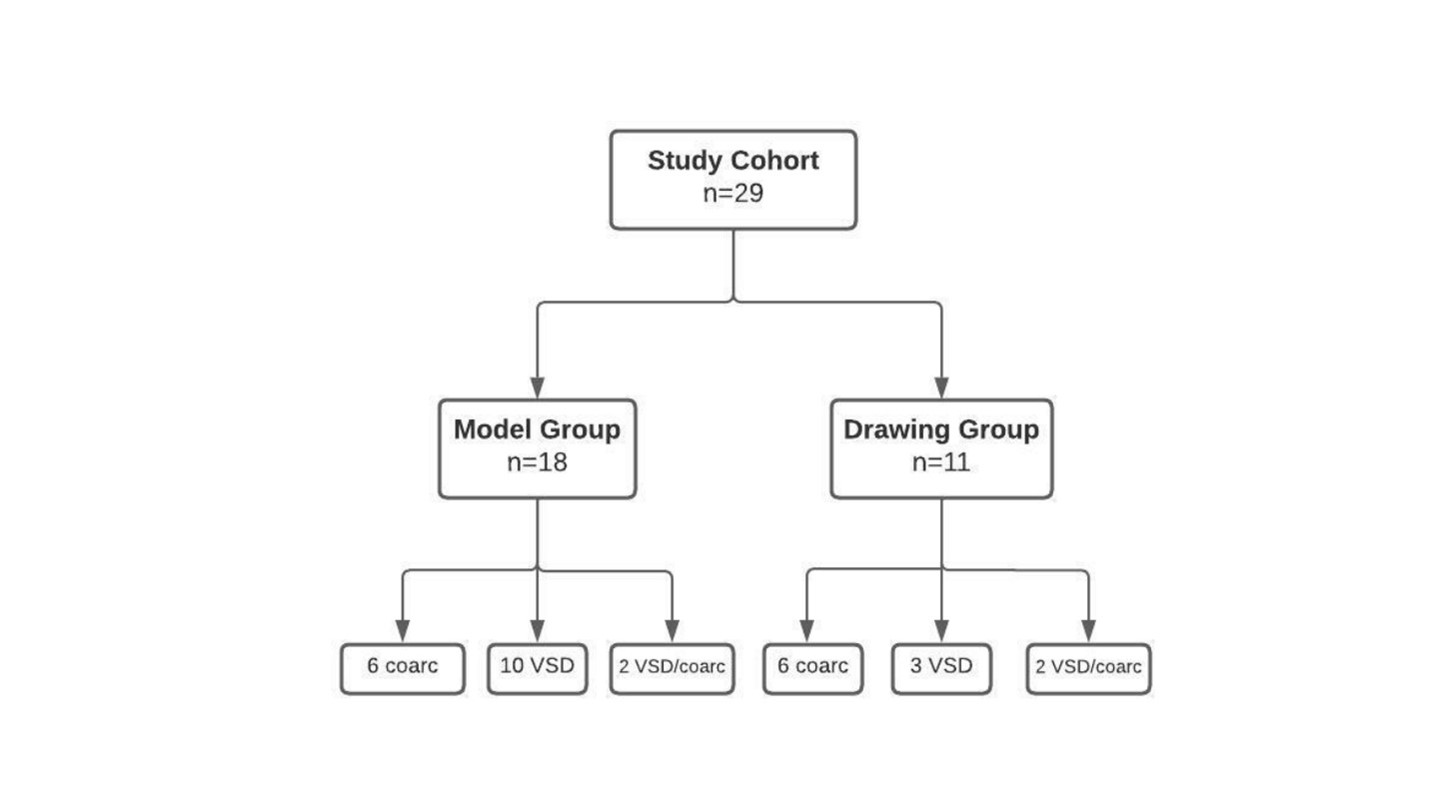
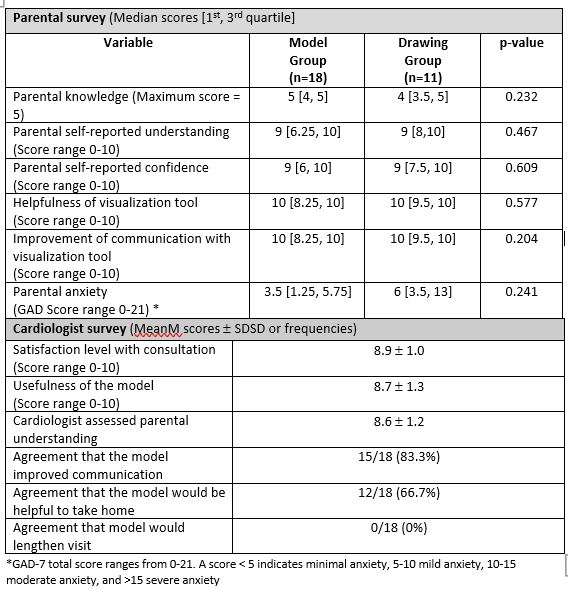
Twenty-nine patients were enrolled over a 12-month period (Figure 2). Both Model and Drawing groups scored similarly in self-reported understanding and confidence, helpfulness of and improvement in communication with the visualization tool. The Model group had higher gross scores on specific questions related to the CHD anatomy and potential surgical intervention (5 [4-5] vs. 4 [3.5-5]), p=0.23 although this did not reach statistical significance. The cardiologists who performed counseling with the 3D models reported high levels of satisfaction with the overall consult and usefulness of the model. After the majority (83%) of consultations, the cardiologist agreed that the 3D model improved communication (Table 1).
Conclusion(s):
This pilot study demonstrates the feasibility of 3DP cardiac model use during prenatal CHD counseling. The results related to parental understanding and knowledge with use of 3DP models are equal to and possibly better than the current standard of care. Evaluation of a larger cohort and use of models with complex CHD may increase the ability to detect circumstances in which models best facilitate counseling.