Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 3
651 - Use of Machine Learning Algorithms in Pediatric Sepsis: A Scoping Review
Publication Number: 651.456
Quinney Fu, MD
Pediatric Emergency Medicine Fellow
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background:
Pediatric sepsis in the United States is estimated to have an overall prevalence of 4.4%, with 176,000 hospitalizations annually and an 8.2% mortality rate. It is also one of the leading causes of childhood mortality worldwide, stressing the importance of early diagnosis and goal directed therapy. Machine learning (ML) is an emerging technology that holds promise to improve early diagnosis and predictive risk stratification for a variety of conditions, including sepsis.
Objective:
This scoping review aims to identify the current landscape of literature regarding the application of ML methods for pediatric sepsis.
Design/Methods:
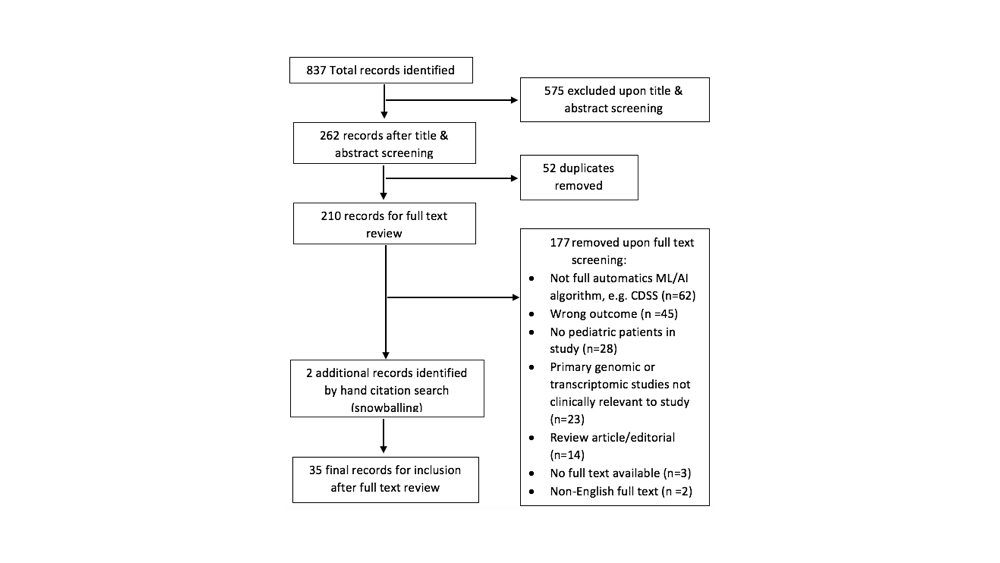
This scoping review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines – scoping review extension (PRISMA-ScR). We used PubMed, CINAHL, Web of Science, and Scopus, and two reviewers independently identified records and screened manuscripts. The search included English language, full-text original research articles published January 2010 onwards that utilized ML or artificial intelligence (AI) for pediatric sepsis diagnosis, early detection, risk stratification, or mortality predication.
Results:
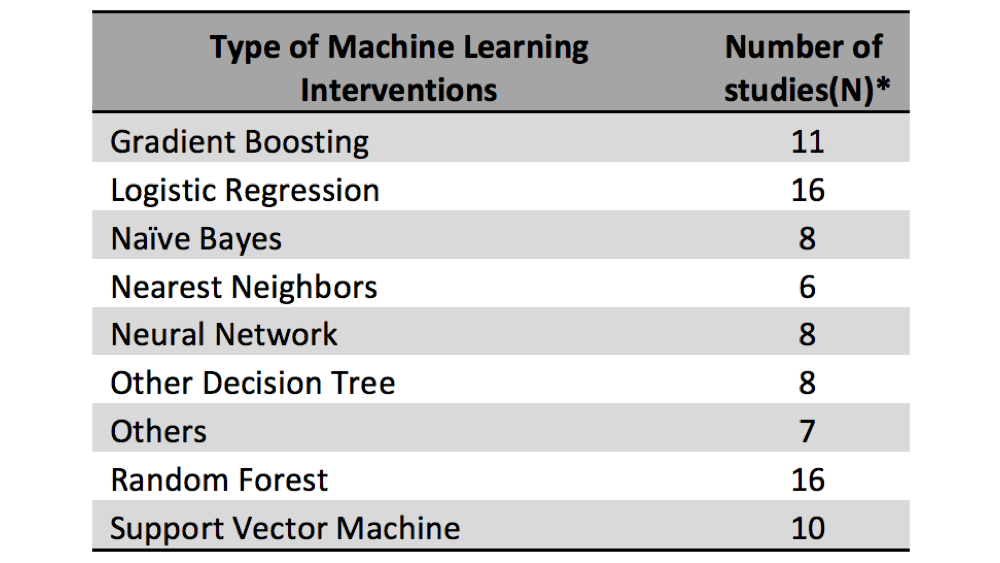
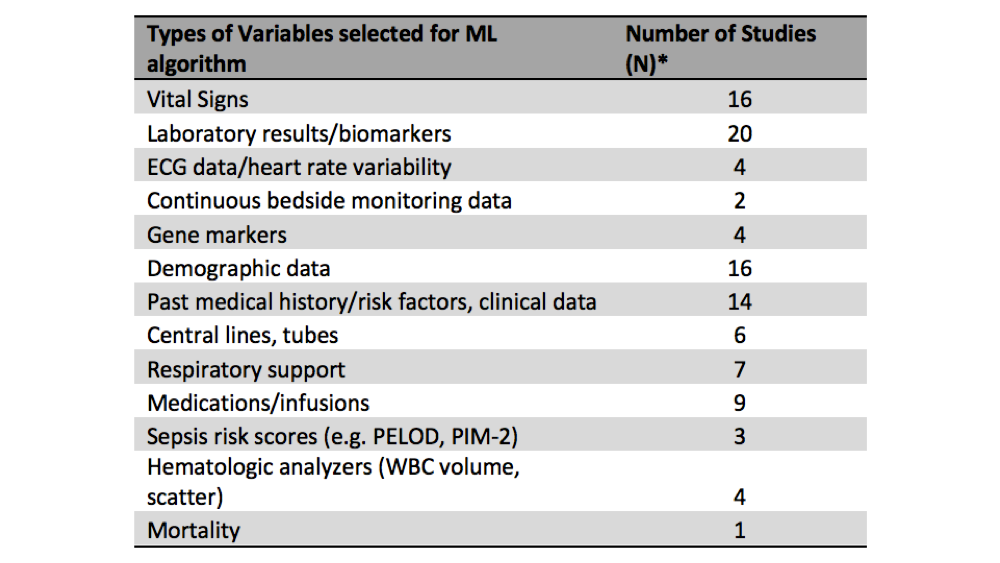
210 records (of 837 screened) were eligible for full text review. Of these articles, a total of 35 were included in the final review. Most of the included studies were retrospective in nature (77%, n = 27), and developed models using datasets from a single institution or health care organization (66%, n = 23). The care setting for the majority of the studies evaluated was the PICU (46%, n = 16) or NICU (37%, n =13), with only 2 studies focusing on the Emergency Department. The most prevalent outcome of interest was risk stratification (e.g. progression to severe sepsis, septic shock, vasoactive medication use), with 13 studies defining this as a primary outcome.
Conclusion(s):
ML research is becoming more prevalent in pediatrics. Age-adjusted-normal for vital signs and physiologic differences make the pediatric sepsis population uniquely challenging for application of ML. While many studies show promise in this area, more multi-center, externally validated and prospective studies are required to provide higher quality evidence to assess suitability for clinical application. Additionally, more attention should be paid to non-intensive care populations such as inpatient, ED and prehospital care settings.