Hospital Medicine: Systems/Population-based Research
Hospital Medicine 5
748 - Predicting Central-Line Associated Bloodstream Infection Risk Using Unit-Level Factors at a Children’s Hospital
Publication Number: 748.414
Peter J. Volkert (he/him/his)
Medical Student
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background:
Central-Line Associated Bloodstream Infections (CLABSIs) are the most common hospital-acquired condition in children and represent the costliest healthcare-associated infection at almost $46,000 per event. Nearly all CLABSIs are preventable with adherence to bundle guidelines for central line management and achieving a reduction in a hospital's CLABSI rate is contingent on excellent staff compliance with these guidelines. Although CLABSI prevention depends on staff efforts, previous risk assessment and CLABSI prediction models have focused on patient-specific factors whereas there are few studies assessing CLABSI risk based on unit- or hospital-wide metrics.
Objective:
The objective of this study was to develop and validate CLABSI risk prediction models using unit- or hospital-wide factors at a Midwest children’s hospital from 2019-2022.
Design/Methods:
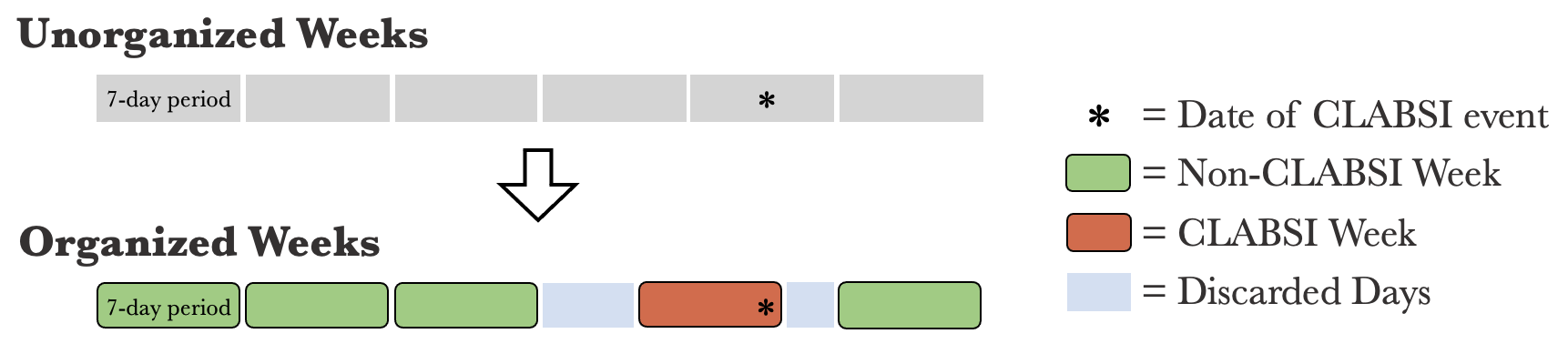
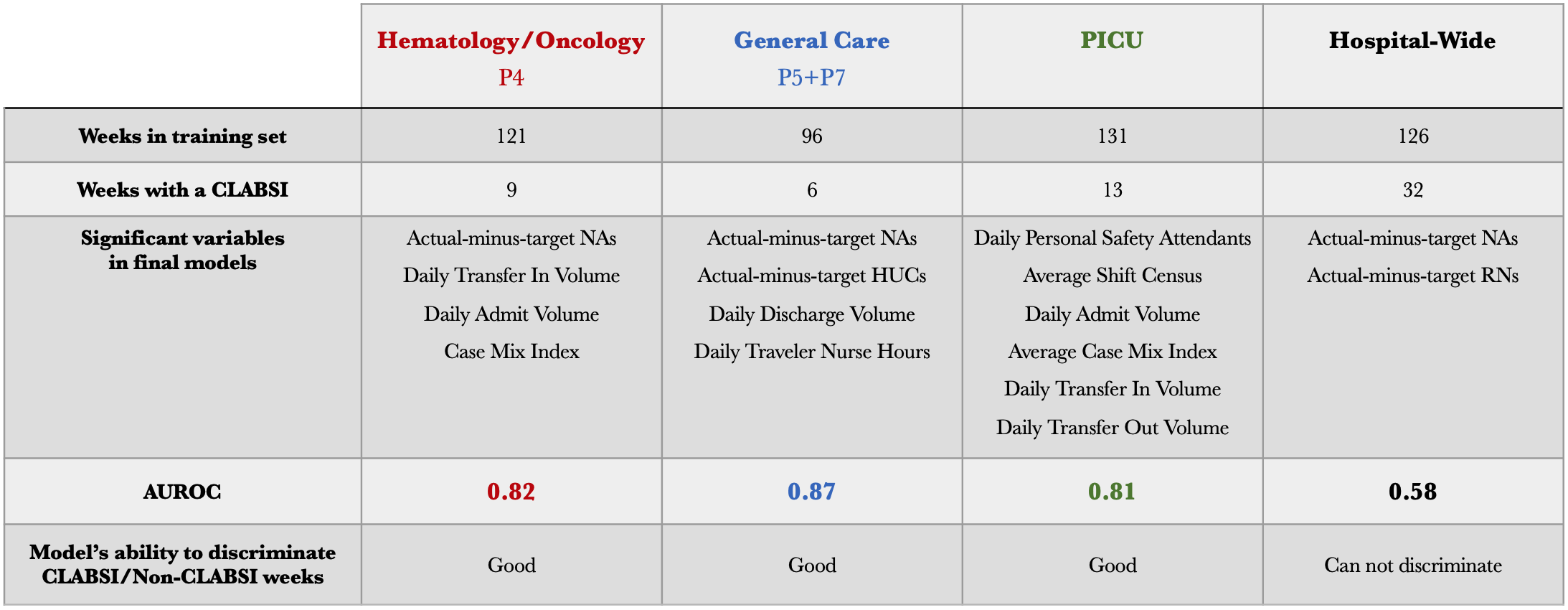
We developed three unit-specific models (P4 - hematology/oncology, P5/P7 - general care, and PICU) and a hospital-wide model to predict weekly CLABSI risk based on 11 daily metrics. Data from March 2019 through December 2021 were used to create the models and data from January 2022 through April 2022 were used for model validation. To create the model, we performed logistic regression analyses of the daily averages of administrative and nurse staffing data for the seven-day period preceding each reported CLABSI. Weeks without a CLABSI were defined as the remaining non-overlapping seven-day periods (Figure 1). Significant variables for each model were determined using stepwise bidirectional elimination. Model performance was evaluated with Area Under the Receiver Operating Characteristic curve (AUROC). We then applied these models to CLABSI events in 2022 to test their predictive ability.
Results:
A total of 37 CLABSIs occurred during the 165 weeks analyzed. Variable selection identified a unique set of risk factors for each model (Figure 2). The predictive power of each of the three unit-level models was considered good (AUROC 0.81 to 0.87), but the hospital-wide regression model was considered non-predictive (AUROC=0.58).
Conclusion(s):
We demonstrate the possibility of using unit-specific weekly data to predict CLABSI risk in a children’s hospital. Differing significant variables for each model indicate that CLABSI risk factors likely differ between hospital units. Variables analyzed in this study were not sufficient to reliably predict CLABSI risk on a hospital-level basis. This study illustrates the possibility that weekly administrative and staffing trends may play a role in CLABSI risk, independent of patient-specific factors.