Infectious Diseases
Infectious Diseases 3
402 - Adaptive Immune Function and Immunoparalysis in Children With Septic Shock
Publication Number: 402.417

Diego A. Cruz Vidal, MD (he/him/his)
Fellow
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
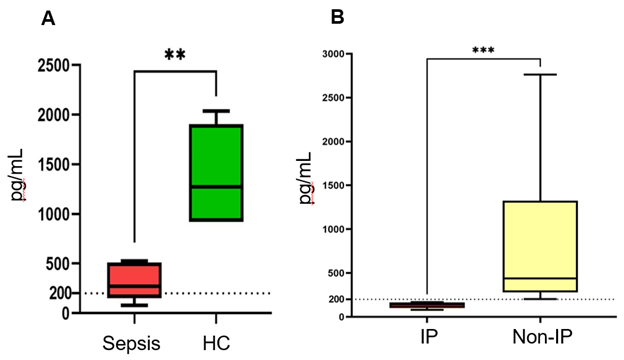
Background: Children with sepsis experience a compensatory anti-inflammatory response that when severe is termed immunoparalysis. In children, immunoparalysis is defined by severe reduction in innate immune function (whole blood ex vivo LPS-induced TNFα production capacity < 200 pg/ml). Adaptive (lymphocyte) immune function is poorly understood in this setting.
Objective: We hypothesize that septic children with immunoparalysis will have concurrent suppression of lymphocyte cytokine production capacity.
Design/Methods:
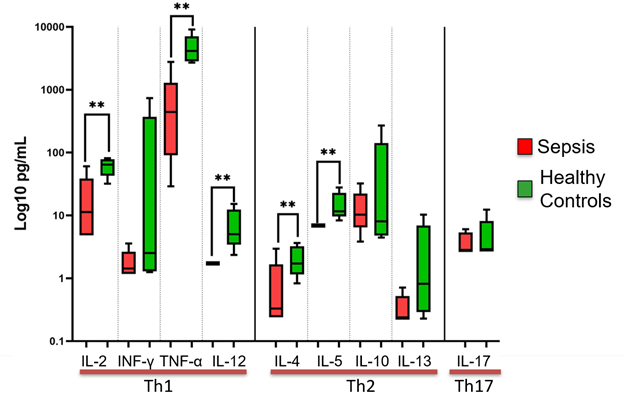
This single-center, prospective, observational study is open to children < 18 years old, excluding those with leukopenia due to myeloablative therapy. Subjects are enrolled and sampled within 48 hours of septic shock onset. Whole blood is stimulated with 500 pg/ml LPS for 4 hrs at 37°C and TNFα is measured in the supernatant. Additional whole blood aliquots are stimulated with 10 µg/ml phytohemagglutinin (PHA, a lymphocyte stimulant) for 24 hrs at 37°C and interleukin (IL)-2, IL4, IL5, IL10, IL12, IL13, IL17, IFNγ, and TNFα are measured in the supernatants. Identical sampling and processing were done in a cohort of healthy control children. Data represents median (IQR).
Results:
16 children with septic shock (age: 15 [8-16] years, 58% male, PRISM III score: 9 [6-12]) and 6 healthy controls (age: 7 [5-9] years, 67% male) have been enrolled. Among septic subjects, 12% had baseline immunocompromise, 56% received hydrocortisone. Ex-vivo TNFα production capacity was lower in children with septic shock vs healthy controls (272 vs 1273 pg/mL), and 6 (38%) had immunoparalysis (Fig 1-A, B).
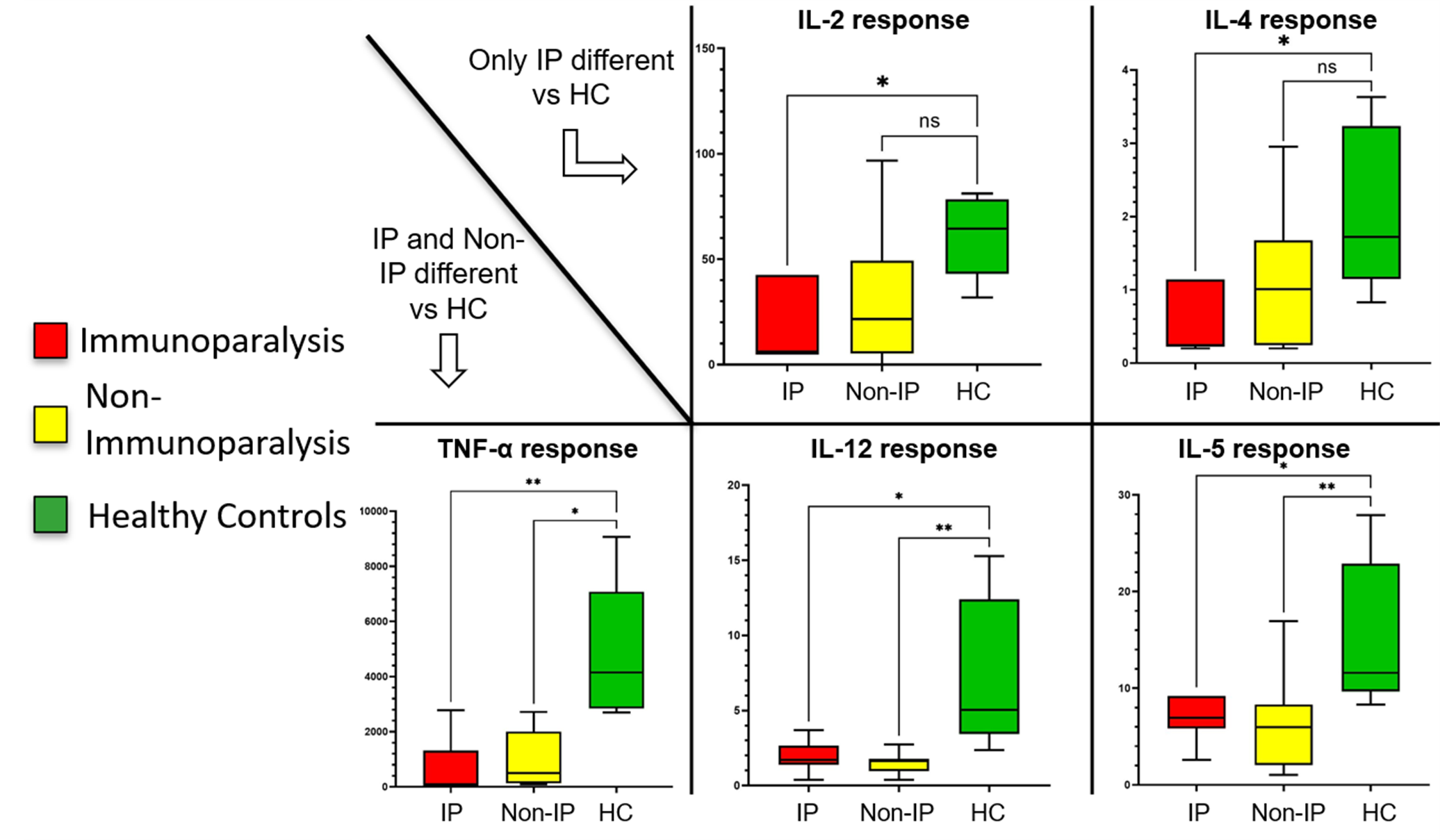
Ex vivo PHA-induced cytokine production was significantly lower in subjects with sepsis vs healthy control for IL2, TNFα, IL12, IL4, and IL5 (Fig 2). The cytokine production capacity was lower in subjects with immunoparalysis vs healthy controls for IL2, IL4, IL5 (6.9 vs 12 pg/ml, p=0.009), IL12, and TNFα. Subjects with sepsis but without immunoparalysis had lower ex vivo PHA-induced production capacities for IL5, IL12, and TNFα vs healthy controls (Fig 3).
Conclusion(s):
Immunoparalysis in septic children is associated with suppression of both innate and adaptive immune responses. PHA-induced cytokine production capacity seems to be decreased in children with septic shock without skewing towards a particular T-cell phenotype. Patients with immunoparalysis may have a different profile of decreased PHA-induced cytokine production capacity. This approach could be used to drive enrollment into future clinical trials of immunomodulatory therapies aimed at restoring adaptive immune function in septic children.