Hospital Medicine: Clinical
Hospital Medicine 6
752 - Concordance Between EHR-recorded Race/Ethnicity and Parental Report in Hospitalized Children
Publication Number: 752.415

Kim Hoang, MD (she/her/hers)
Clinical Assistant Professor
Stanford University School of Medicine
San Mateo, California, United States
Presenting Author(s)
Background: Electronic health records (EHRs) have become an important repository for patient race and ethnicity. This has allowed hospitals and researchers to better identify and characterize health disparities. However, because race and ethnicity are complex constructs, and due to a lack of a standardized approach to solicit this information, the EHR may not accurately portray parents’ real-time self-report of their child’s race/ethnicity. Misclassification could negatively affect efforts to monitor and reduce health disparities.
Objective: We assessed the concordance of parental report of race/ethnicity for their hospitalized child with EHR documented demographics. We also aimed to describe parents’ preferences on how race/ethnicity should be captured in the hospital’s EHR.
Design/Methods:
From December 2021 to May 2022, we conducted a single-center cross-sectional survey of parents of hospitalized children less than 18 years old. We asked parents to describe their child’s race/ethnicity and compared these responses to the race/ethnicity documented in the EHR. Concordance was analyzed with a kappa statistic (k). Additionally, we queried respondents about their awareness of and preferences for race/ethnicity documentation and described these responses using proportions and 95% confidence intervals.
Results:
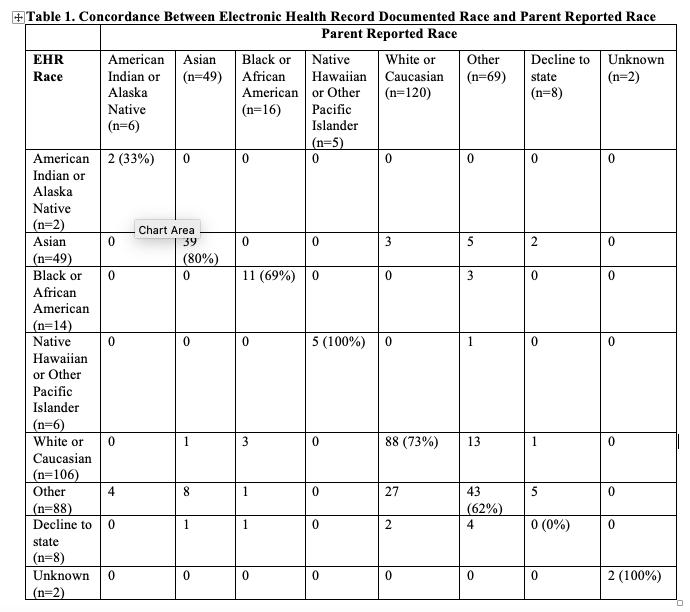
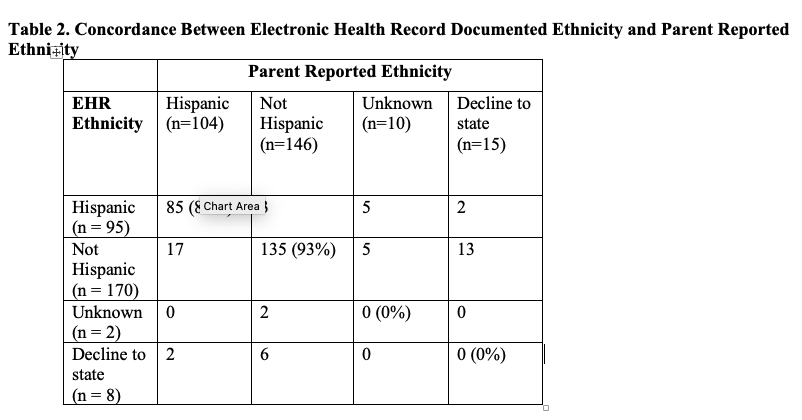
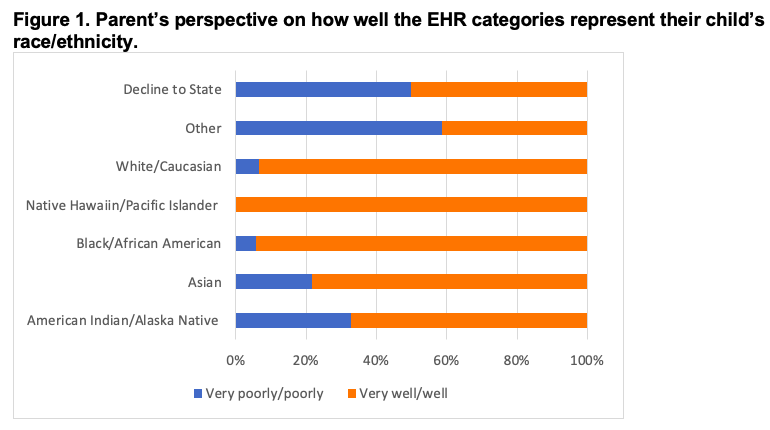
Of the 275 participants surveyed (79% response rate), there was 69% agreement (k=0.56, weak concordance) for race and 80% agreement (k=0.63, moderate concordance) for ethnicity. Table 1 and 2 illustrates the concordance for each race and ethnicity. Sixty-eight parents (21%) felt that the designated categories poorly represent their child’s race/ethnicity, though this proportion was higher for specific racial groups (p < 0.01, Figure 1). Fifty-five (20%) respondents were not aware their child’s race/ethnicity was displayed in the EHR. Twenty-two (8%) were uncomfortable with their child’s race/ethnicity being displayed on the hospital’s EHR. Eighty-nine (32%) preferred more comprehensive, multiselect race/ethnicity lists and 34 (12%) preferred a free text box.
Conclusion(s): Non-concordance between EHR-recorded race/ethnicity and parental report exists in the EHR for our hospitalized patients which has implications for describing patient populations and for understanding racial and ethnic disparities. Current EHR categories may be limited in their ability to capture the complexity of these constructs. Future efforts should focus on ensuring that demographic information in the EHR is accurately collected and appropriately reflects families’ preferences.