Cardiology
Cardiology 3
719 - Socioeconomic determinants of Prenatal Diagnosis of Tetralogy of Fallot (ToF) and Long-Term Imaging Surveillance of ToF following Repair
Publication Number: 719.4

Elena Tsemberis, BA (she/her/hers)
Medical Student
George Washington University School of Medicine and Health Sciences
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Children with repaired Tetralogy of Fallot (rTOF) benefit from surveillance with cardiac magnetic resonance (CMR) imaging to identify cardiac dysfunction requiring surgical intervention. Socioeconomic (SES) and geographic factors barriers may prevent timely receipt of CMR; this effect in rTOF patients has not been studied.
Objective:
We aimed to assess an association of SES and race/ethnicity on access to CMR utilization and biventricular function in a retrospective cohort of rTOF patients. We compared SES characteristics between patients with a prenatal versus postnatal ToF diagnosis.
Design/Methods:
rTOF patients >2 years of age referred for CMR from 2010-2021 were compared against concurrent surgical cohort of rTOF patients < 2 years of age. The surgical cohort served as control, representing patients receiving standard short-term care. Self-reported race, ethnicity and addresses were collected. Census tract software cdxzipstream extracted census tract characteristics and a composite SES score was derived, using 6 variables representing wealth, income, education, and occupation. Measurements of function including left and right ventricular ejection fraction (LVEF, RVEF) as well as SES characteristics including number of MRI studies, and prenatal versus postnatal diagnosis, within the CMR cohort were collected.
Results:
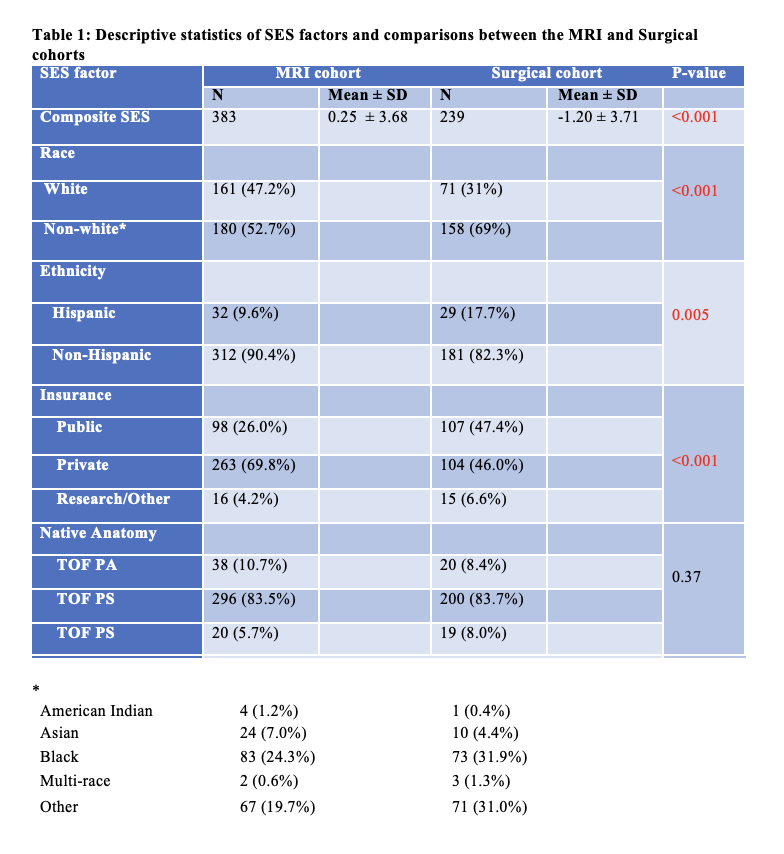
There were differences in SES and demographics between CMR cohort (n=383) and surgical cohort (n=239) (Table 1). The CMR cohort lived in areas with less poverty, higher median income and higher composite SES score (p< 0.001). The CMR cohort had more white patients and non-Hispanic patients (p< 0.001, p=0.005). The CMR cohort had a greater proportion of privately insured patients (p< 0.001).
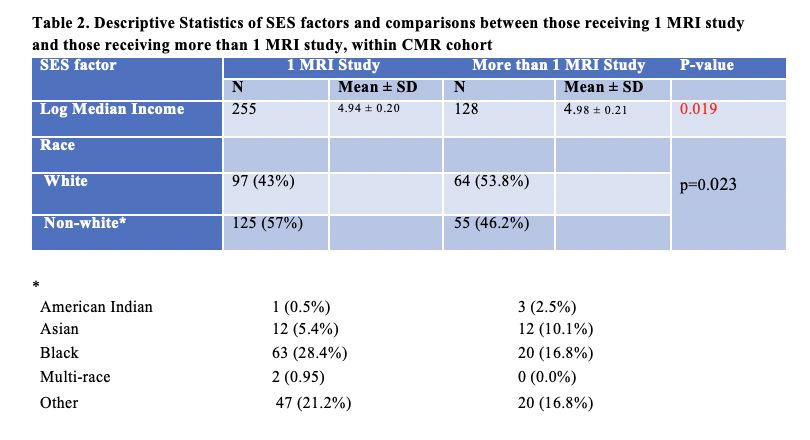
Disparities were found within the CMR cohort. Patients with LV dysfunction (LVEF < 55%, a late finding in rTOF) lived in areas with more poverty (p=0.043), lower median income (p=0.008) and lower composite SES score (p=0.005). Patients who received >1 MRI study lived in areas with a higher median income than those who received 1 MRI study (p=0.019). More white patients and fewer Black patients received >1 MRI study (p=0.023) (Table 2). In the surgical cohort, patients who were diagnosed prenatally lived in areas with more poverty than those diagnosed postnatally (p=0.019).
Conclusion(s):
CMR utilization and metrics of cardiac function may have SES and racial disparities in rTOF patients. The results have implications in healthcare equity and long-term outcomes for this population of patients. Further study is needed to identify the underlying mechanisms.