Neonatal Pulmonology
Neonatal Pulmonology 4: Exosomes, Stem Cells, Maternal and Fetal Environmental Effects
142 - Preeclampsia alters tracheo-alveolar fluid proteomic angiogenic profile in extremely premature infants
Publication Number: 142.436
.jpg)
Veronica Caballero, MD (she/her/hers)
Fellow
University of Miami Leonard M. Miller School of Medicine
Miami Springs, Florida, United States
Presenting Author(s)
Background:
Extremely preterm infants born to mothers with preeclampsia (PE) have a higher risk of severe RDS and BPD. PE is associated with disrupted fetal lung angiogenesis but the persistence of the anti-angiogenic milieu in the preterm lung and its impact on respiratory outcome have not been well defined.
Objective:
To determine if PE is associated with alterations in the tracheo-alveolar fluid (TAF) angiogenic profile in preterm infants and to determine if these alterations are associated with worse respiratory outcome.
Design/Methods:
TAF was collected on day 1 (d1) from intubated infants of 23-28 w gestation admitted to the NICU at Holtz Children’s Hospital of the University of Miami/Jackson Memorial Medical Center. Angiogenic factors were measured by multiplex assay and normalized to protein concentration. Respiratory outcomes included total days on O2 and FiO2 at 36 w PMA. Analysis was done by Mann-Whitney U Test or T-Test . The relationship between d1 angiogenic factors and respiratory outcome was modeled using Generalized Estimating Equations.
Results:
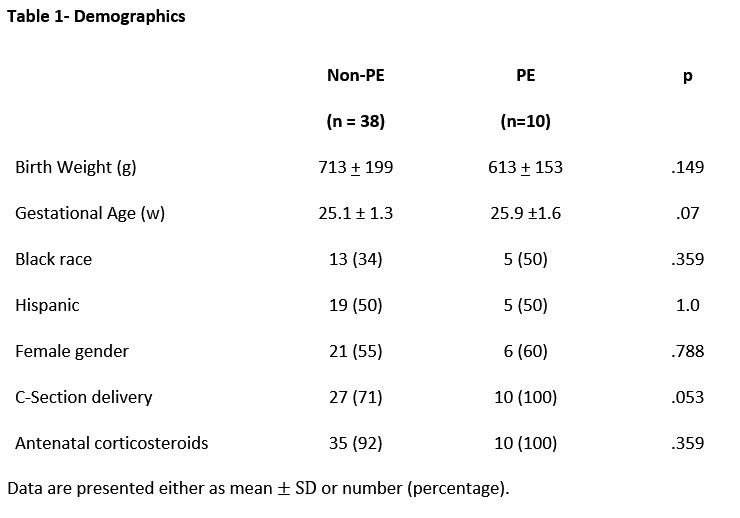
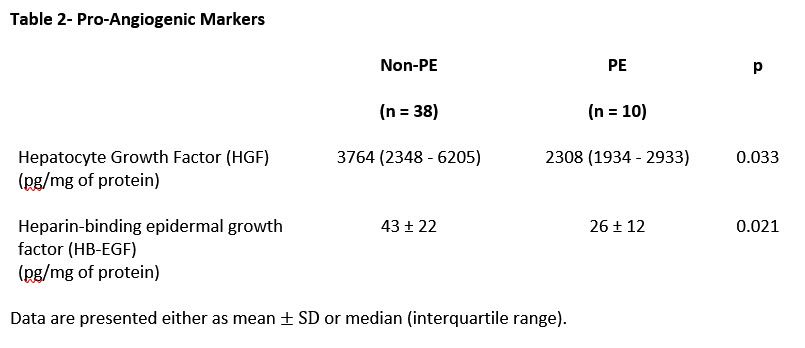
The cohort included 48 infants of whom 10 were born to mothers with PE. Demographics are shown in Table 1. Pro-angiogenic factors hepatocyte growth factor (HGF) and heparin-binding epidermal growth factor (HB-EGF) were decreased in the PE compared to the non-PE group (Table 2). Other factors including angiopoietin-2, bone morphogenetic protein-9, epidermal growth factor, endoglin, fibroblast growth factor-1, fibroblast growth factor 2, follistatin, granulocyte colony stimulating factor, interleukin-8, leptin, and vascular endothelial growth factors A, C and D did not differ.
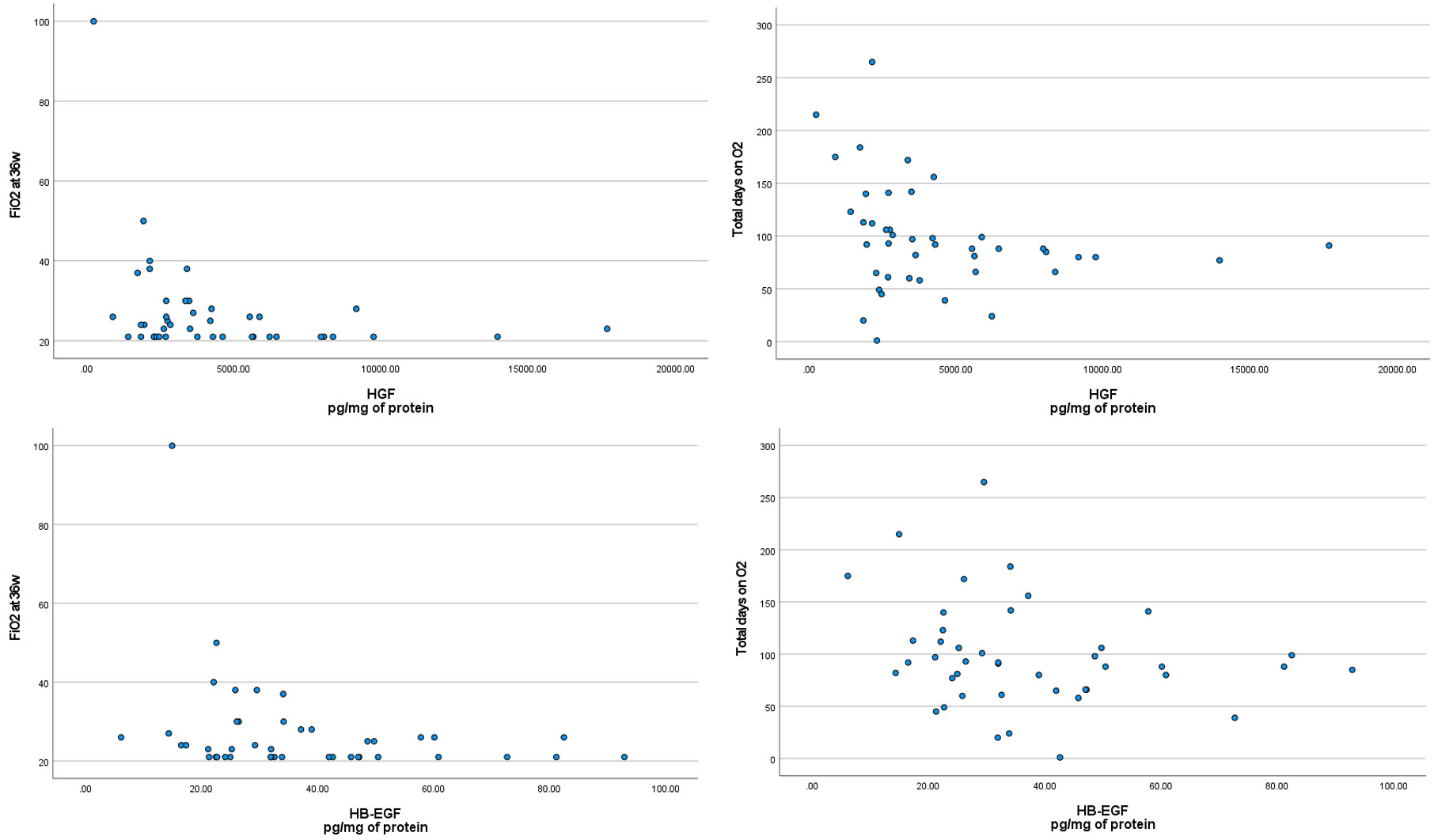
Lower d1 HGF levels were associated with longer O2 duration [beta: -.004 (CI: -.007, -.001), p=.022]. There was a trend towards higher FiO2 at 36w PMA with lower d1 TAF levels of both HGF [beta: -.001 (CI: -.002, 0.000086, p=.07] and HB-EGF [beta: -.141 (CI: -.303, .021), p=.07]. Figure 1 shows the relationship between d1 HGF and HB-EGF with FiO2 at 36 w PMA and supplemental O2 duration.
Conclusion(s):
Pro-angiogenic factors in TAF of preterm infants born to mothers with PE were decreased and this was associated with prolonged O2 dependency. This suggests persistence of the anti-angiogenic environment that can impact respiratory outcomes. The mechanisms by which these alterations affect lung development need to be examined. Supported by NHLBI grants (U01 HL133689, UO1 HL133708).