Infectious Diseases
Infectious Diseases 3
412 - Parents’/Patients’ Communication with Primary Care Providers on MenB Vaccination for Older Adolescents and Young Adults in the United States
Publication Number: 412.417

Diana E. Clements, MD
Medical Director
GSK
Philadelphia, Pennsylvania, United States
Oscar Herrera-Restrepo, PhD (he/him/his)
US Health Outcomes Director
GSK
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
Background:
The Advisory Committee on Immunization Practices recommends vaccination against invasive meningococcal disease (“meningitis” in this study) caused by serogroup B (MenB) for healthy 16–23-year-old adolescents and young adults based on shared clinical decision-making (SCDM) between patients/parents and providers. However, this recommendation based on SCDM may be unclear to patients/parents and providers.
Objective:
This study assessed how parents of 16–18-year-old adolescents (PoA) and how 19–23-year-old young adults (YA) communicated with their primary care provider (PCP) regarding MenB vaccination.
Design/Methods:
PoA and YA from the United States (US) were randomly recruited from a US-based patient panel in Sept–Oct 2022. Participants completed an online survey regarding their conversations with PCPs about MenB vaccination. Adolescent children of PoA and YA had received ≥1 dose of the MenB vaccine (Figure 1).
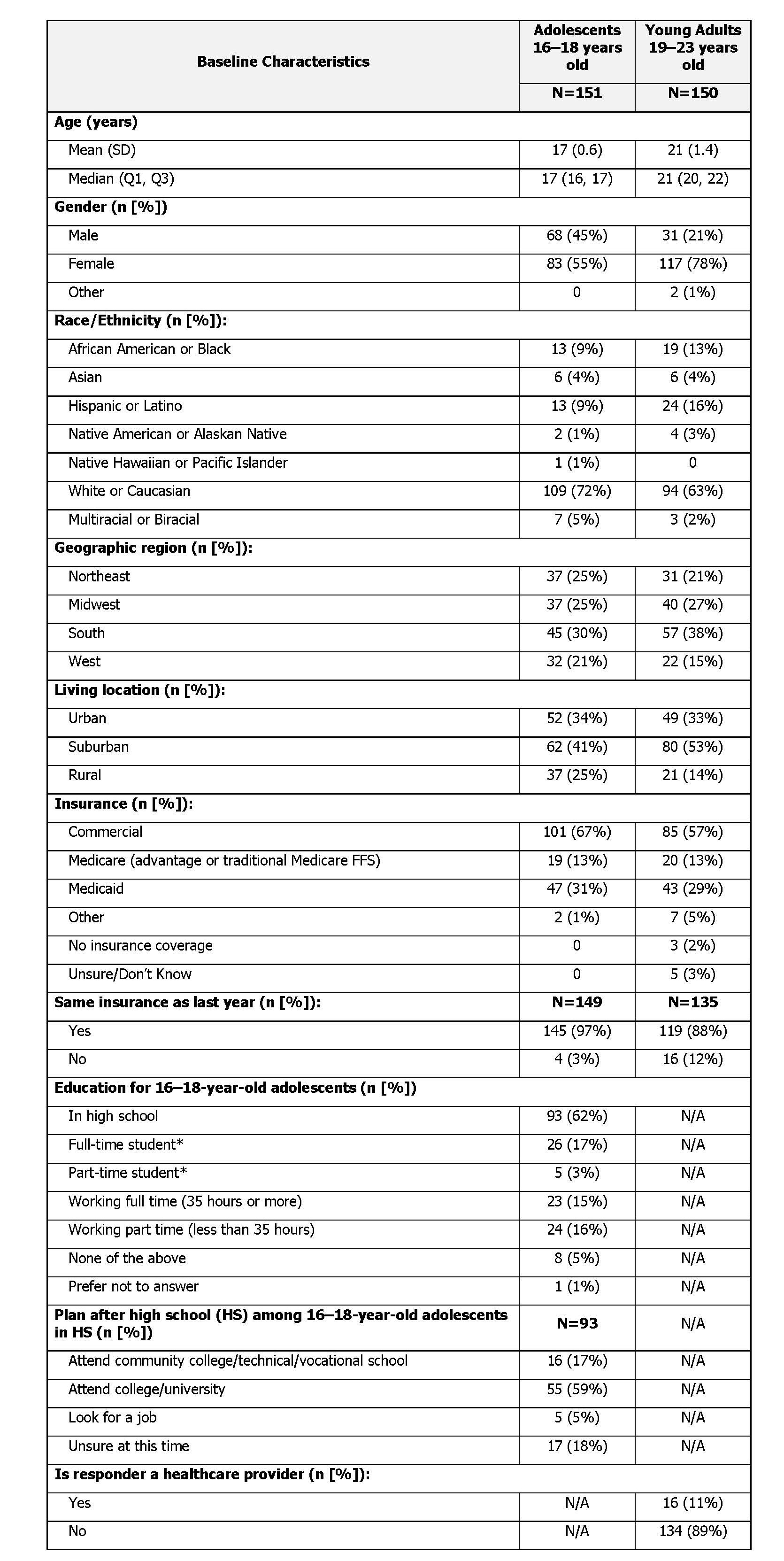
Results: A total of 301 participants were included (151 PoA and 150 YA; Table 1). Most discussions on the MenB vaccine were reported to have been initiated by PCPs (74% PoA, 62% YA); only 20% of PoA and 15% of YA reported initiating these conversations. The top reason for participants to initiate the MenB conversation was school/college requirement (57% PoA, 53% YA). Over half of PoA (76%) and YA (61%) considered their PCP to be responsible for MenB vaccination initiation; only 13% of YA held their parents responsible. The conversation lasted < 10 min for 63% of PoA and 59% of YA. The importance of vaccination was the main discussion topic for most participants (67% PoA, 52% YA). Most PoA (65%) and YA (55%) reported not being aware of what SCDM is. Many PoA (44%) and YA (61%) reported moderate-to-low PCP effort in providing MenB vaccine information. PCPs were described as having strongly recommended the vaccine by 52% of PoA and 38% of YA. By contrast, 20% of PoA and 36% of YA described the PCPs’ recommendation as a consideration, mentioning benefits and noting that the decision was up to the patients. Lastly, 69% of PoA and 52% of YA reported getting the vaccine right after the conversation at the office/clinic (Table 2).
Conclusion(s): SCDM is variably implemented in the primary care setting; many PoA and YA are not aware of their role in vaccine discussions. These findings suggest that if conversations are not initiated by PCPs, patients/parents may not have access to appropriate vaccine information. Targeted patient/parent and medical education on SCDM may provide more opportunities to ensure access to information on MenB vaccination. 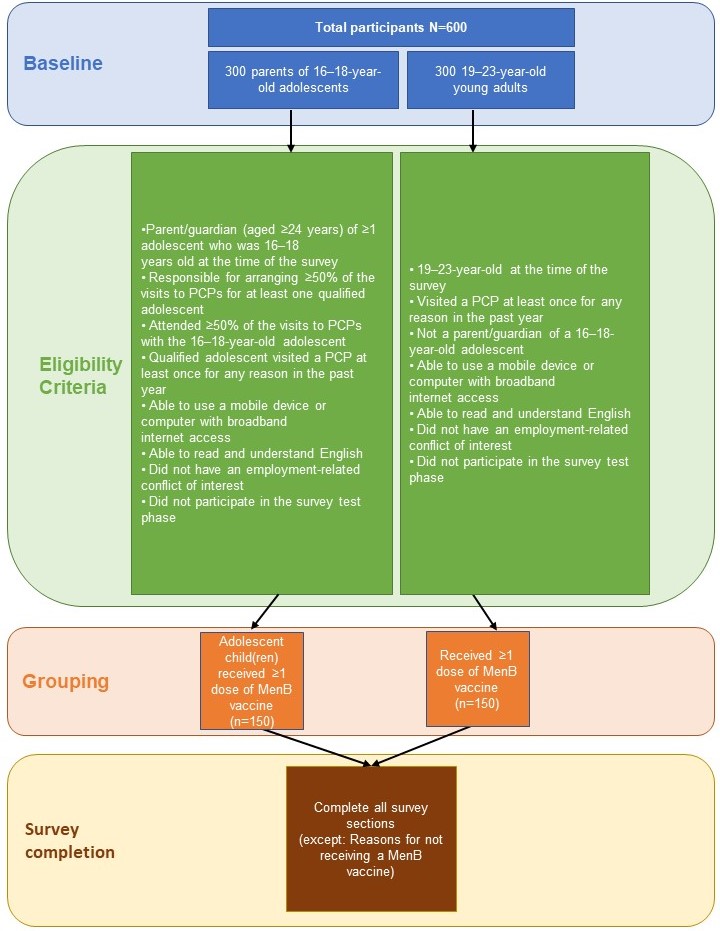
.jpg)
