Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
671 - Factors associated with failure of initial non-invasive respiratory support in late preterm and term infants and its impact on outcomes
Publication Number: 671.443
- BH
Bethany L. Hunt (she/her/hers)
Medical Student
Rutgers, Robert Wood Johnson Medical School
Piscataway, New Jersey, United States
Presenting Author(s)
Background:
Late preterm and term infants commonly receive non-invasive respiratory support (N-IRS) after birth with a small proportion of them failing and requiring escalation of this support. In contrast to extremely preterm infants, there are very limited data on the factors associated with this failure and its impact on outcomes.
Objective: To determine the impact of failure of initial N-IRS on in-hospital outcomes and identify risk factors associated with this failure in late preterm and term infants.
Design/Methods:
We conducted a retrospective cohort study of all inborn infants with gestational age (GA) ≥ 34w from 2012-19 at Rutgers Robert Wood Johnson University Hospital who required N-IRS within 12h of birth. Infants with congenital anomalies were excluded.
N-IRS failure was defined as any of the following within 12h of admission: escalation of respiratory support mode, surfactant administration, increase in FiO2 >0.2 above the baseline or absolute value >0.4 for at least 3h.
In-hospital outcomes and perinatal factors were compared between N-IRS failure and N-IRS success groups using Chi-Square for categorical and T test for continuous variables, or nonparametric Mann-Whitney U Test as determined by Shapiro-Wilk test. Multivariate stepwise binary logistic regression (LRA) was used to model the association between demographic and perinatal factors and N-IRS failure.
Results:
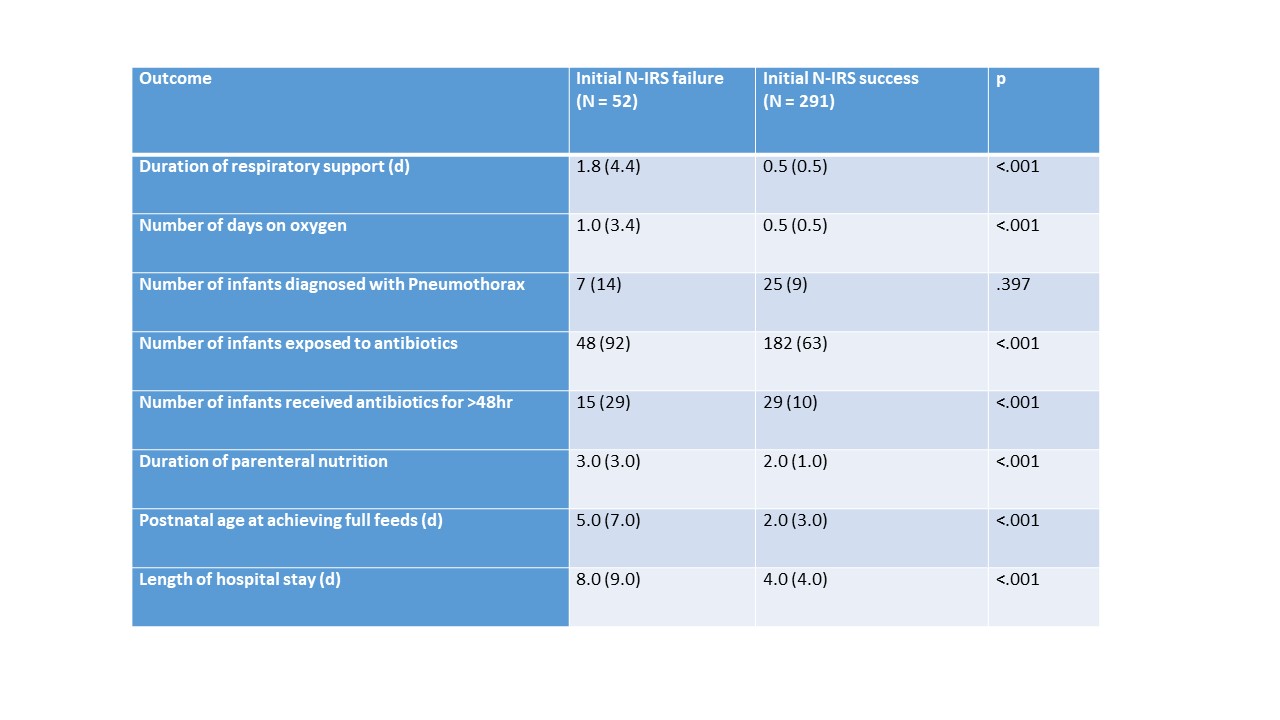
Of 343 eligible infants during the study period, 52 (15%) failed initial N-IRS. Failure group had longer duration of respiratory support [1.8d (4.4) vs 0.5d (0.5), median (IQR); p < .001] and length of stay [8d (9) vs 4d (4), median (IQR); p < .001] as compared to N-IRS success. (Table 1)
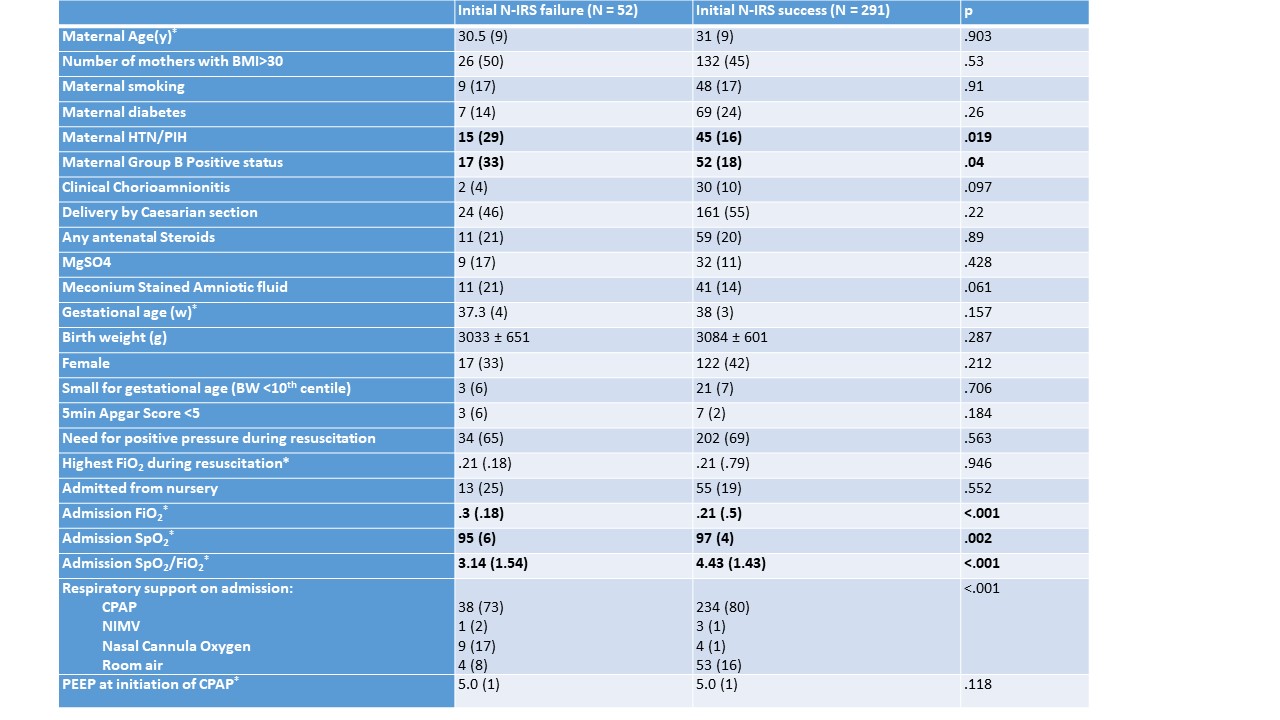
More infants in N-IRS failure group were exposed to maternal hypertension, born to GBS positive mothers. There was no difference in GA, mode of delivery or neonatal resuscitation between the groups. Infants in N-IRS failure group were on higher FiO2 on admission to NICU. (Table 2)
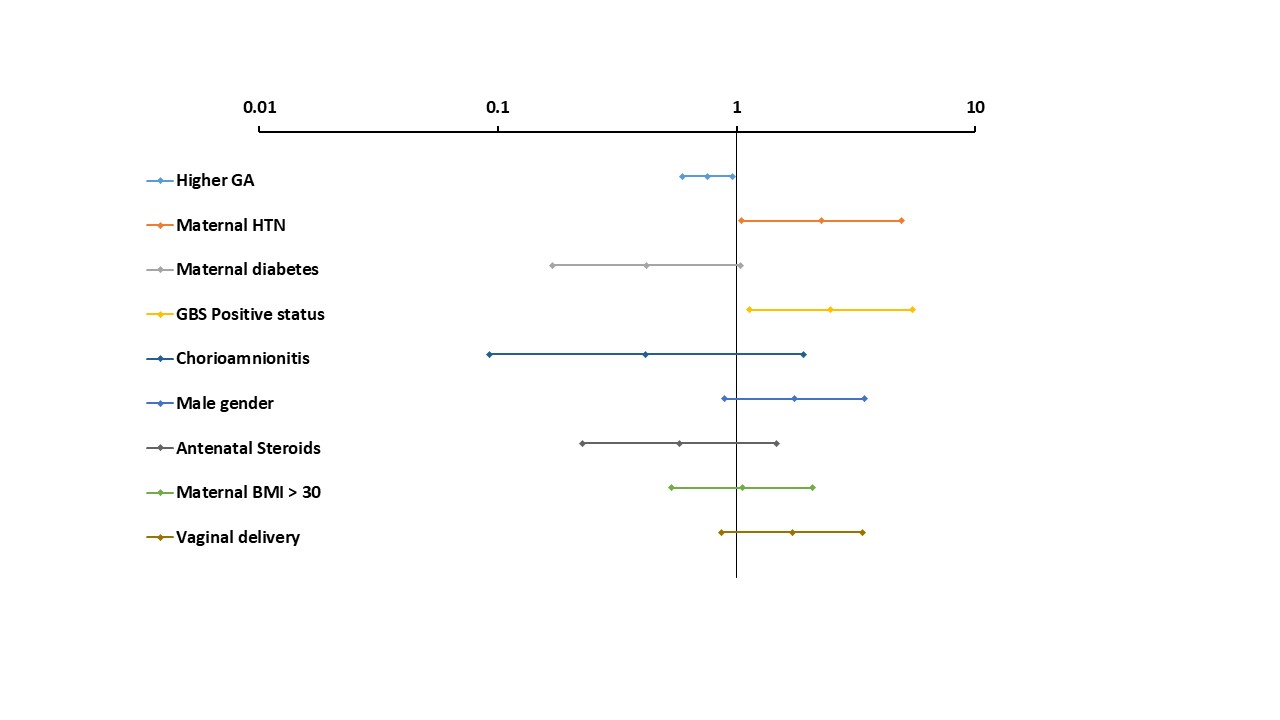
On LRA, maternal hypertension (aOR 2.261 (95% CI 1.044 – 4.894) and positive GBS status (aOR 2.479 ( 95% CI 1.128 – 5.448) were associated with increased odds of failure of N-IRS. (Figure)
Conclusion(s):
Failure of initial non-invasive respiratory support in this population was associated with significantly longer duration of respiratory support, hospital stay and more frequent exposure to prolonged course of antibiotics. Interestingly, maternal hypertensive disorders and GBS positive status were associated with the failure. The pathophysiological basis of these associations and their potential role in prediction of failure of respiratory support need to be further investigated.