Emergency Medicine: All Areas
Emergency Medicine 4
60 - Exploring Unmet Social Needs and Interest in Community Resource Referral during Pediatric Emergency Department Visits
Publication Number: 60.112

Natalie J. Tedford, MD (she/her/hers)
Pediatric Emergency Medicine & Global Health Fellow
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
The practice of social needs screening is extending to pediatric emergency departments (PEDs), but there is limited understanding of how unmet social needs (USN) are then addressed in this evolving practice.
Objective:
To examine and describe USNs across demographics of a pilot social needs screening and referral program in a PED and explore interest in referral to a community resource center
Design/Methods:
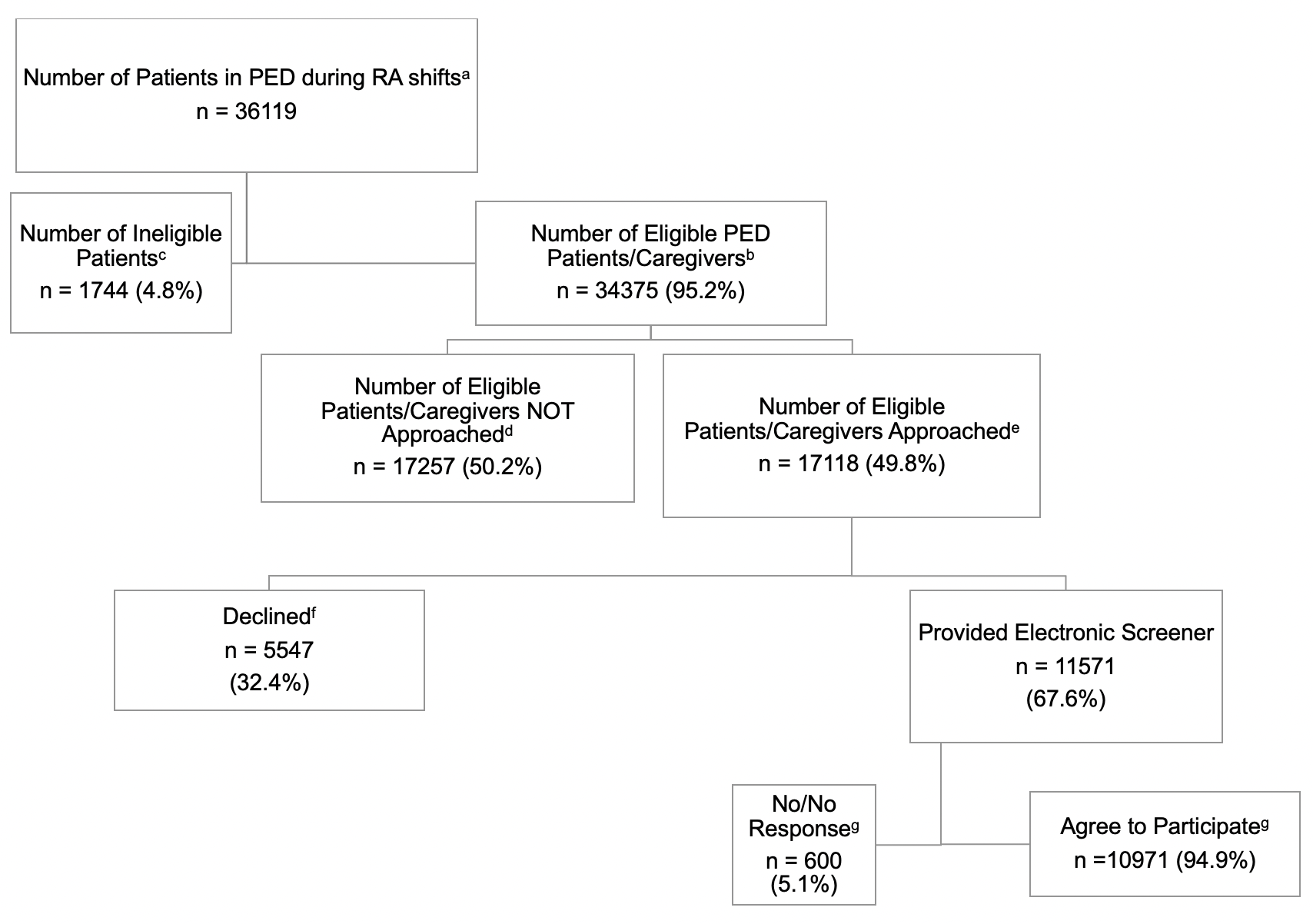
This was a cross-sectional, analytical study in a PED at a quaternary level children’s hospital. Research assistants (RA) approached English- and Spanish-speaking caregivers of patients < 18 years of age. Each enrolled caregiver was offered a pediatric version of the validated Screener for Intensifying Community Referrals for Health (p-SINCERE). In the caregiver’s preferred language, the survey assessed 10 areas of social needs and self-reported demographics and asked if referral to United Way 211 was desired. All caregivers who opted-in to referral are contacted by a resource specialist from United Way 211 within 48 hours to link families to resources. Outcomes of interest were prevalence of USN and interest in 211-referral. We summarized and compared variables between self-selected language using descriptive statistics.
Results:
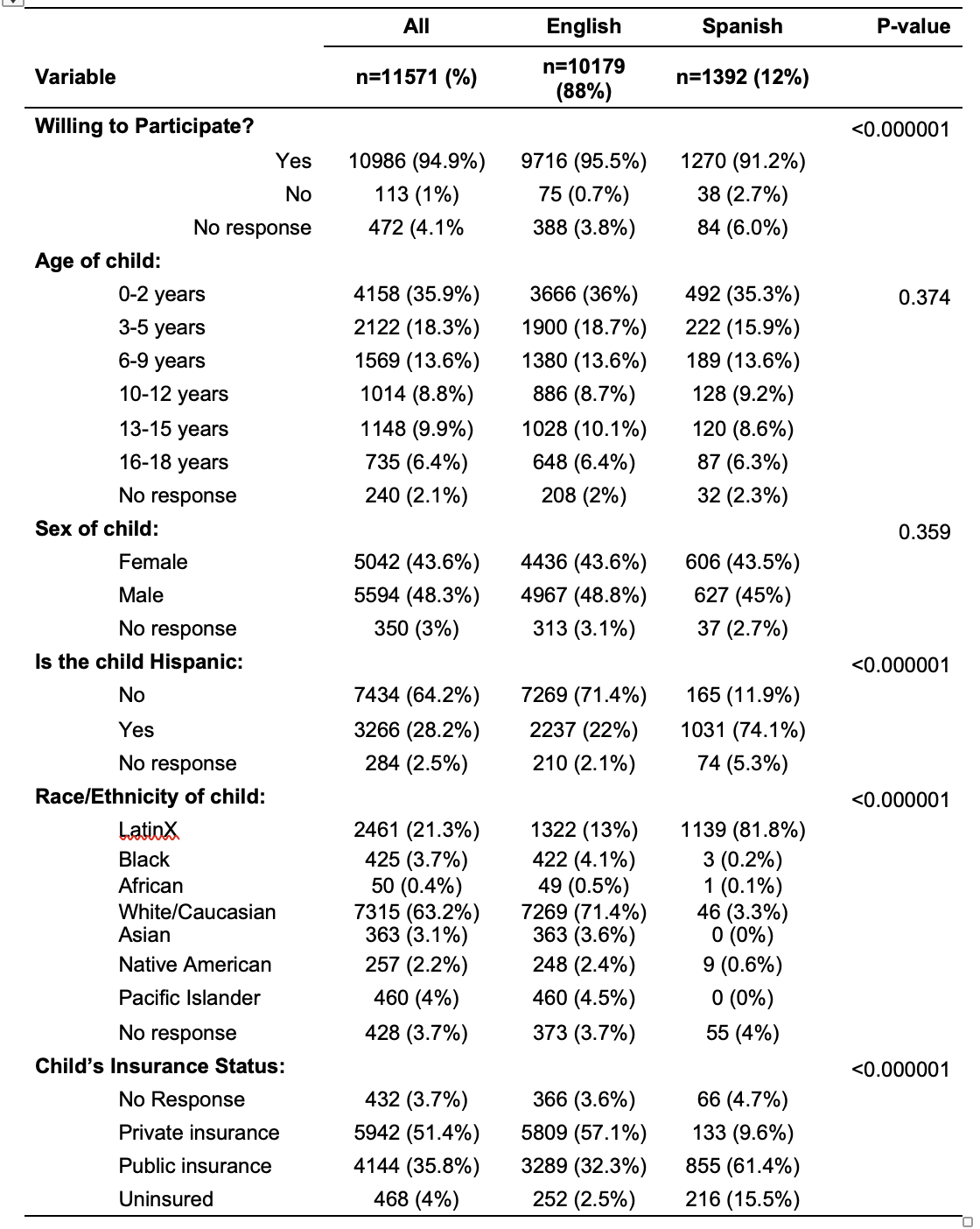
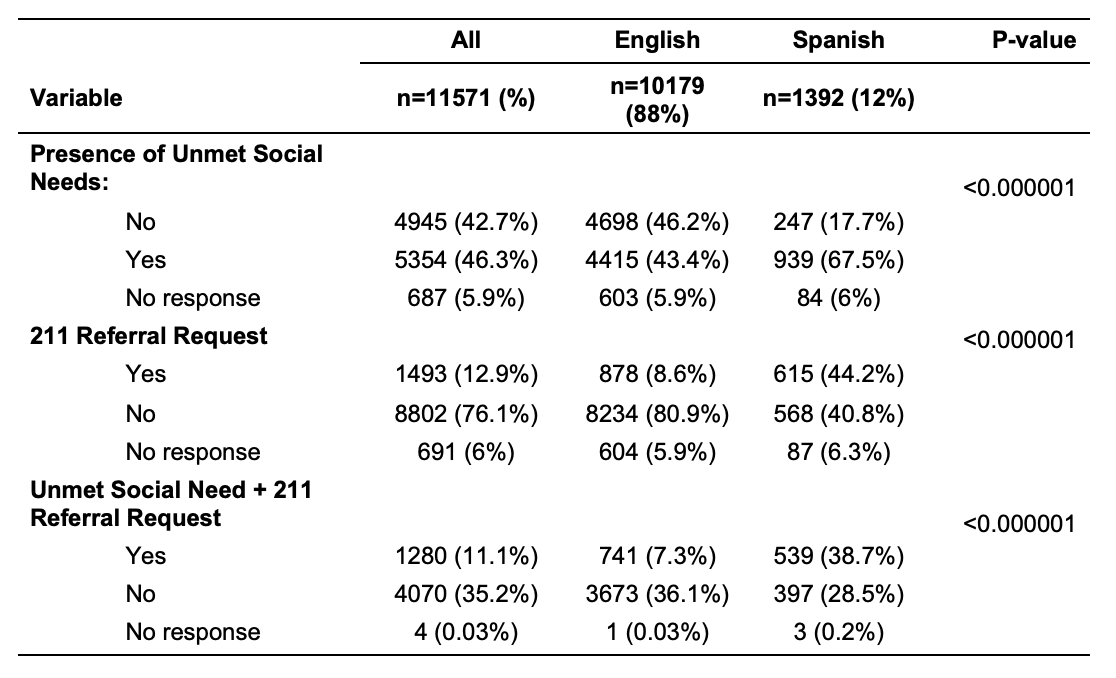
From 09/27/21 to 12/7/22, 11571 caregivers were provided an electronic screener with preferred language noted English for 10179 (88%) and Spanish for 1392 (12%) (Figure 1). Enrolled patients were mostly male (48.3%), non-Hispanic (64.2%), White/Caucasian (63.2%), had private health insurance (51.4%), had an English-speaking caregiver (88%), had ≥1 USN (46.3%), and did not request 211 referral (76.1%) (Table 1&2). There were 5342 caregivers reporting ≥1 USN (46.3%), representing 43.4% of English-speaking caregivers and 67.5% of Spanish-speaking caregivers (p < 0.0001) (Table 2). There were 1492 caregivers requesting referral to 211 (12.9%), representing 8.6% of English-speaking caregivers and 44.2% of Spanish-speaking caregivers (p < 0.0001) (Table 2).
Conclusion(s):
Although USNs are common among patients/caregivers in a PED, presence of USN does not equate to caregiver requesting community resource referral. The disparities present in historically marginalized populations is evident in our sample and highlights the need for processes in healthcare settings, including the PED, that help to mitigate the negative systemic impacts faced by these populations.