Hospital Medicine: Clinical
Hospital Medicine 7
769 - Effect of saline concentration of maintenance intravenous fluids in pediatric patients admitted with gastroenteritis
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 769
Publication Number: 769.416
Publication Number: 769.416
Anisha Kesarwani, Cohen Children's Medical Center, Manhasset, NY, United States; Abby Basalely, N/A, New Hyde Park, NY, United States; Laura Castellanos, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New Hyde Park, NY, United States; Pamela Singer, Cohen Children's Medical Center, Cedarhurst, NY, United States; Rachel Frank, Cohen Children's Medical Center, Jericho, NY, United States; Christine Sethna, Cohen Children’s Medical Center, New Hyde Park, NY, United States
- AK
Anisha Kesarwani, MD (she/her/hers)
Pediatric Resident
Cohen Children's Medical Center
Manhasset, New York, United States
Presenting Author(s)
Background: Administration of hypotonic intravenous fluids (IVF) was previously standard practice in pediatrics until concerns were raised that hypotonic IVF led to increased cases of hospital-acquired hyponatremia. In 2018, the American Academy of Pediatrics released guidelines recommending the use of isotonic fluids for maintenance IVF in children. However, isotonic IVF have their own potential risks.
Objective: To determine the effect of switching from hypotonic saline to isotonic saline administration as maintenance IVF on clinical measures and hospital outcomes in children admitted with gastroenteritis.
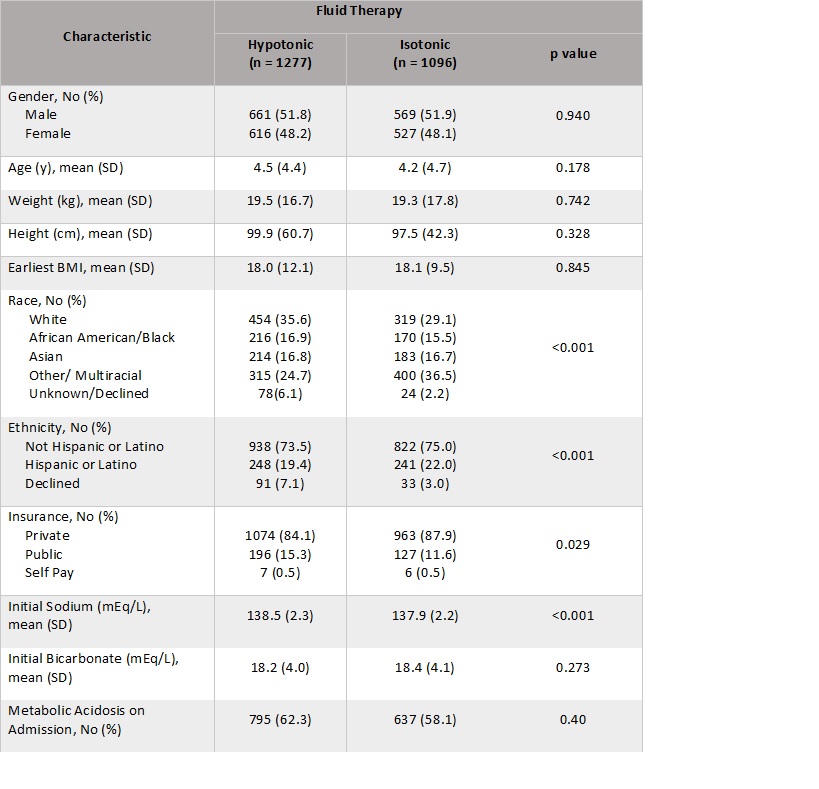
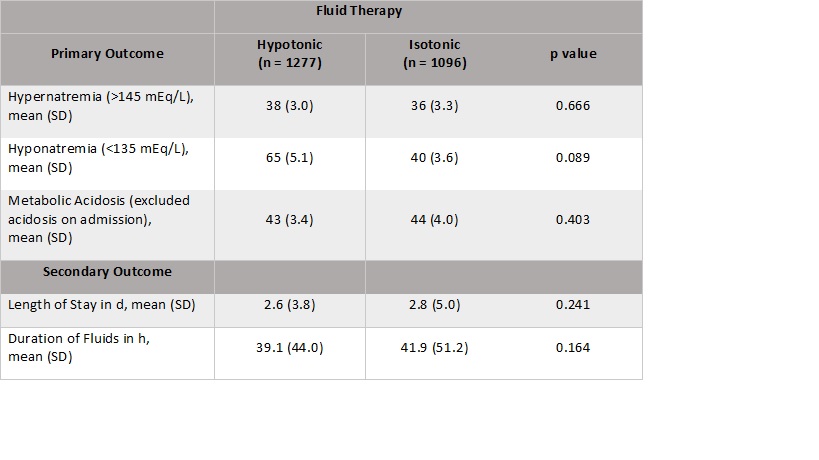
Design/Methods: A retrospective chart review was performed on children aged 2 months-18 years admitted to the general pediatrics floor for gastroenteritis at a tertiary children’s hospital. Children who required maintenance IVF and were isonatremic on presentation were included. Children with major comorbid illness or who were admitted to the intensive care unit were excluded. Data were analyzed from 1/1/2013-12/31/2015, the time period prior to the institution of isotonic IVF usage, and 1/1/2018-12/31/2020, the time period post implementation of isotonic IVF as standard practice. Primary outcomes were the proportion of children who developed hypernatremia (serum sodium >145 mEq/L), hyponatremia (serum sodium < 135 mEq/L) or metabolic acidosis (serum bicarbonate < 20mEq/L). Secondary outcomes were length of hospital stay and duration of IVF. T-tests and chi-square compared outcomes by time period. Linear and logistic regression models adjusted for age, sex and insurance type examined the relationship between IVF time period and outcomes.
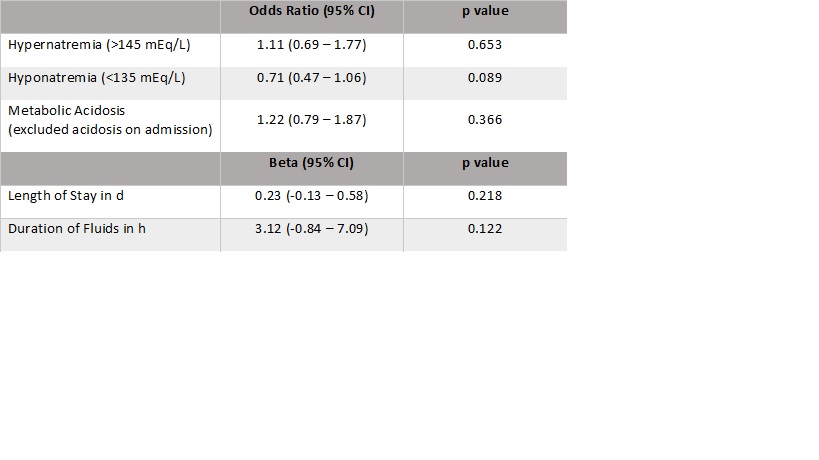
Results: There were 1277 patient visits during the hypotonic IVF era and 1096 patient visits during the isotonic IVF era. Compared to the hypotonic IVF group, the isotonic IVF group self-identified less as White, more as Hispanic, had less public insurance, and had a lower serum sodium level on admission (Table 1). There was no significant difference in the number of patients who developed hypernatremia, hyponatremia, or metabolic acidosis between groups. Length of stay and duration of fluids were also not significantly different between the two IVF groups (Table 2). In adjusted regression models, there was no association between IVF group and any outcome (Table 3).
Conclusion(s): Contrary to expectation, there was no difference in the incidence of electrolyte abnormalities, duration of IVF administration or hospital length of stay during the hypotonic IVF era compared to isotonic IVF era.