Emergency Medicine: All Areas
Emergency Medicine 13
364 - Impact of Race on Triage in the Pediatric Emergency Department
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 364
Publication Number: 364.404
Publication Number: 364.404
Prisca Takundwa, Yale-New Haven Children's Hospital, Hamden, CT, United States; Connor V. Haynes, Yale School of Medicine, New Haven, CT, United States; Veronika Shabanova, Yale University, New Haven, CT, United States; Sarah McCollum, Yale University School of Medicine, Department of Pediatrics, New Haven, CT, United States; Melissa L. Langhan, Yale university, New Haven, CT, United States

Prisca Takundwa, MS, MD (she/her/hers)
Clinical Fellow, Pediatric Emergency Medicine
Yale-New Haven Children's Hospital
Hamden, Connecticut, United States
Presenting Author(s)
Background: Disparities exist in the healthcare delivered to racial and ethnic minorities. Many Emergency Departments (EDs) use standardized scoring systems to triage patients according to illness severity, which should allow for equitable and appropriate use of resources. One such score is the emergency severity index (ESI), where a lower score indicates higher acuity (e.g., level 2 is “Emergent”, and level 5 is “non-urgent”).
Objective: To evaluate whether pediatric patients presenting to an ED receive different ESI scores for identical chief complaints based on their perceived race/ethnicity. It is our hypothesis that the race/ethnicity of the patient influences this scoring system.
Design/Methods: A prospective cross-sectional study was conducted among pediatric ED triage nurses in an urban academic hospital. Using ESI triage criteria and in consultation with nurse and simulation educators, sixteen standardized patient cases were created along with an internal control case. Each case included a name and picture of four patients of different race/ethnicity: Caucasian, African American, Asian, and Hispanic. The patients were randomly assigned for each subject. Subjects were asked to assign an ESI level for each of the sixteen cases.
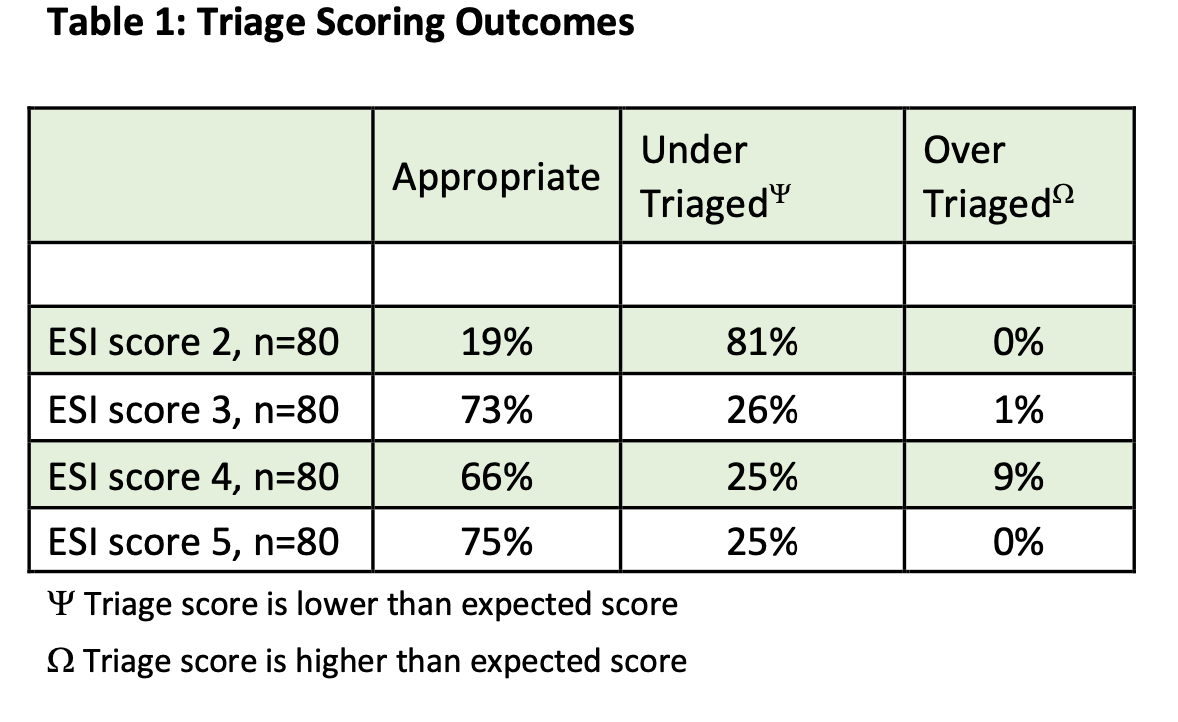
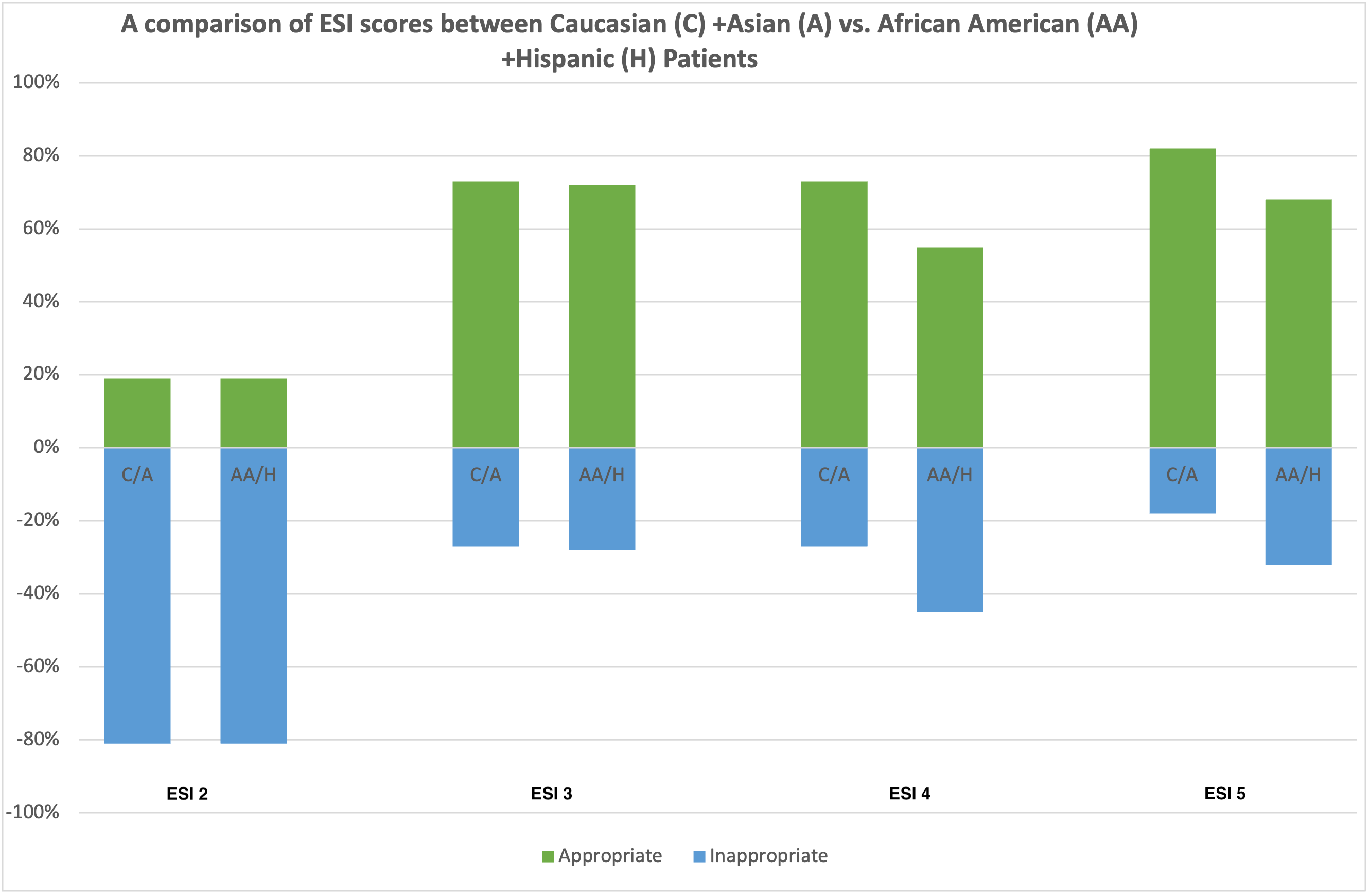
Results: Twenty-two nurses have participated to date; 95% were female and 100% identified as Caucasian. The internal control case was appropriately assigned by 62% of subjects. Table 1 shows the percent of subjects who correctly and incorrectly triaged the cases by ESI level. A large percentage of ESI 2 cases (81%) were triaged at a lower level, whereas the majority of ESI 3, 4 and 5 cases were assigned the correct level. Figure 1 shows the differences in ESI scores by race/ethnicity categories. There were no statistically significant differences in ESI scores between Caucasian and Asian compared to African American and Hispanic patients (ESI 2 p=0.97, ESI 3 p=0.89, ESI 4 p =0.09, and ESI 5 p=0.16)
Conclusion(s): There is concordance in expected triage score to actual score given with lower acuity chief complaints at ESI levels 3, 4 and 5. Higher acuity patients (ESI 2) were inappropriately triaged across all race/ethnicities. There was no significant difference in triaging between African American and Hispanic patients compared to Caucasian and Asian patients suggesting a lack of unconscious bias in triage of patients presenting to the pediatric ED.