Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
670 - Creating a Novel “CPAP Discontinuation Readiness” Score for Preterm Infants
Publication Number: 670.443

Faith Myers, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background:
Infants born < 32 weeks’ gestation with respiratory distress syndrome (RDS) typically undergo immediate initiation of nasal continuous positive airway pressure (CPAP). CPAP discontinuation may occur once an infant reaches >32 weeks’ post-menstrual age, demonstrates stability on CPAP ≤5 cm H20 with minimal inspired oxygen needs, and exhibits few apnea, bradycardia or desaturation events. However, CPAP weaning failure occurs frequently and is associated with numerous setbacks. A clinical score to aid in predicting successful CPAP discontinuation is necessary to standardize practice and to determine optimal timing of weaning.
Objective:
Identify clinical variables predictive of successful CPAP discontinuation in neonates to create a novel “CPAP Discontinuation Readiness” score.
Design/Methods:
We analyzed medical records of 132 patients with RDS born between 24 and 32 weeks’ gestation admitted to a Level IV neonatal intensive care unit. We collected variables including CPAP level, supplemental oxygen (fiO2), SpO2, heart rate, and number of apnea, bradycardia, or desaturation events within 24 hours prior to CPAP discontinuation. We tested associations between each feature and weaning success with a univariate logistic regression model. Penalized multivariate logistic regression was then used to determine an area under the curve (AUC) to formulate a predictive clinical score.
Results: Between 2020 and 2022, 93 infants met inclusion criteria with 121 CPAP discontinuation attempts. Infants were trialed off CPAP at a mean post-menstrual age of 32 weeks and 5 days on a CPAP level of ≤5 cm H20 for a mean of 10 days. 73 of 93 (78%) of patients were successful on the first CPAP discontinuation attempt (did not require re-application of CPAP interface for 7 days following discontinuation). Several clinical factors including SpO2 (OR 1.30, p=0.001), fiO2 requirement (OR 0.37, p=0.05), and respiratory rate (OR 0.44, p=0.001) within the preceding 24 hours were associated with successful CPAP discontinuation (Figure 1). Number of ABD events was positively associated with CPAP discontinuation success. A clinical score using these variables to predict CPAP weaning success revealed an AUC of ~70% (Figure 2).
Conclusion(s):
Clinical variables including SpO2, fiO2, and respiratory rate are associated with CPAP discontinuation success. A novel “CPAP Discontinuation Readiness” score created using these variables is predictive of successful CPAP discontinuation. This score carries the potential to standardize the practice of CPAP discontinuation and prevent premature discontinuation or prolonged CPAP use in premature infants. 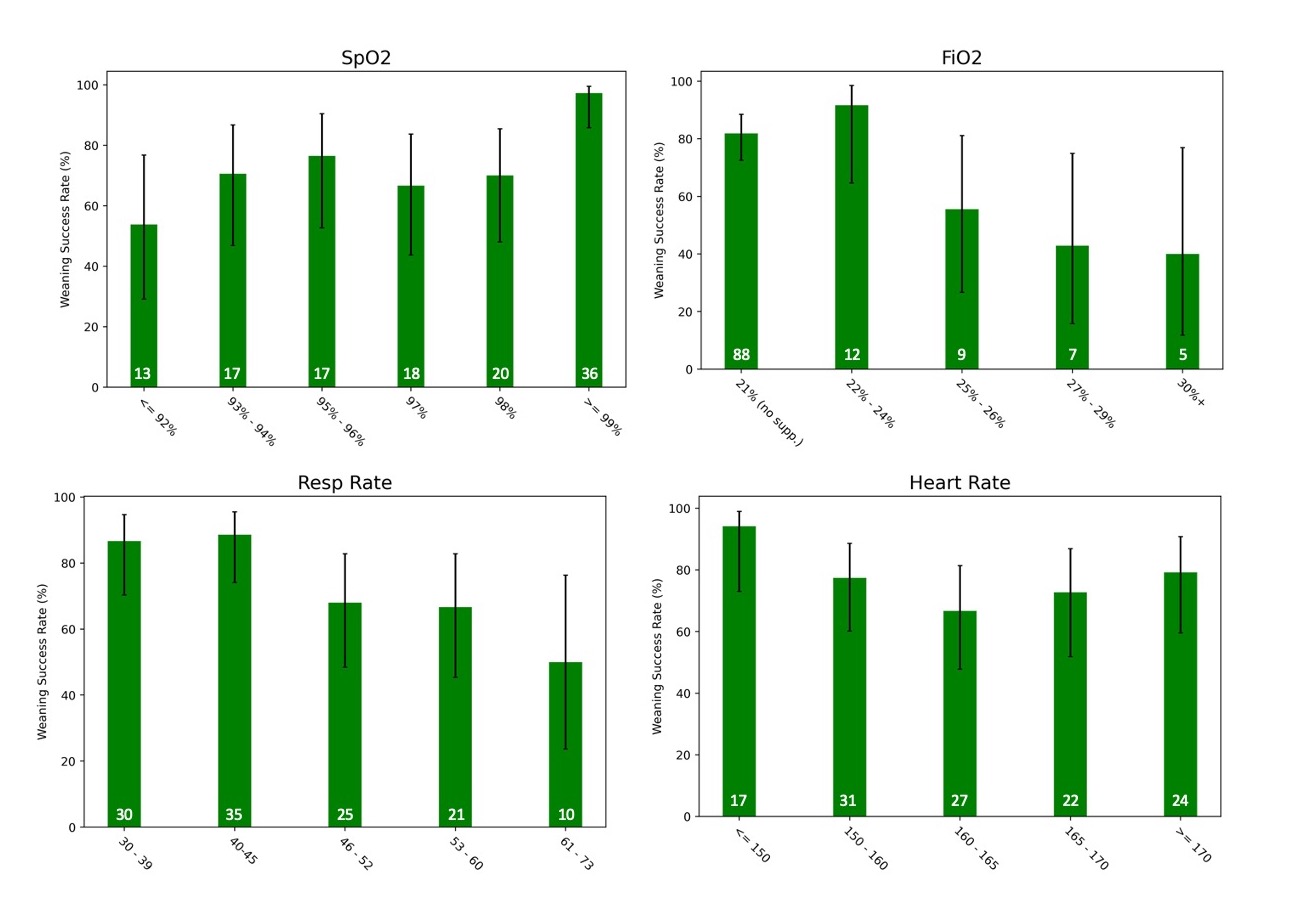
.jpg)
