Medical Education: Resident
Medical Education 13: Resident 4
483 - Resident-Attending Dyads in the Pediatric Emergency Department: A Social Network Analysis
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 483
Publication Number: 483.421
Publication Number: 483.421
Kelsey A. Miller, Boston Children's Hospital, Brookline, MA, United States; Sarah C. Cavallaro, Boston Children's Hospital, Boston, MA, United States; Alexander Hirsch, Boston Children's Hospital, Brookline, MA, United States; Kate Dorney, Boston Children's Hospital, Newton, MA, United States; Michael Monuteaux, Boston Children's Hospital, Boston, MA, United States; Joshua Nagler, Boston Children's Hospital, Brookline, MA, United States
- KM
Kelsey A. Miller, MD, EdM (she/her/hers)
Attending Physician in Pediatric Emergency Medicine
Boston Children's Hospital
Brookline, Massachusetts, United States
Presenting Author(s)
Background: The pediatric emergency department (PED) is a rich source of education for pediatric and emergency medicine residents. PEDs often have a large faculty supervising resident-patient encounters. Large pools of learners and faculty can lead to discordant alignment of clinical ED shifts among residents and attendings, resulting in many possible resident-attending dyads and limiting interactions between a specific resident-attending pair.
Objective: This study aimed to use social network analysis to understand the frequency and intensity of interactions between unique resident-attending dyads in the PED.
Design/Methods: We retrospectively analyzed resident rotations between July 2018 and June 2022, including each rotation for residents rotating multiple times, to identify all patients seen by an individual resident. For each resident-patient encounter, we extracted the resident involvement in the initial evaluation, disposition, or entire ED encounter from timestamps in the electronic health record; we used the same methodology to identify all attendings supervising a resident over the course of a rotation. Using social network analyses, we calculated the degree centrality (number of ties per node) and density (number of observed out of all possible connections) and compared these across residency programs (pediatric versus emergency medicine) and postgraduate year (PGY).
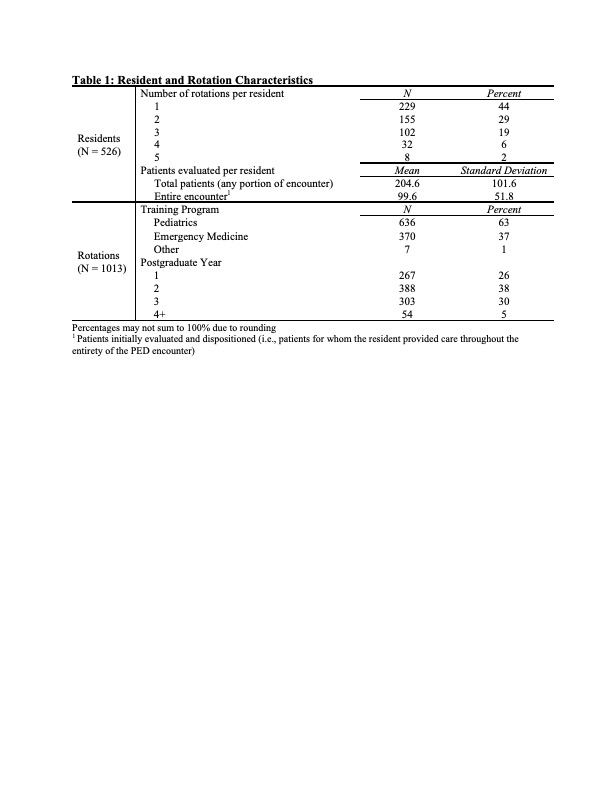
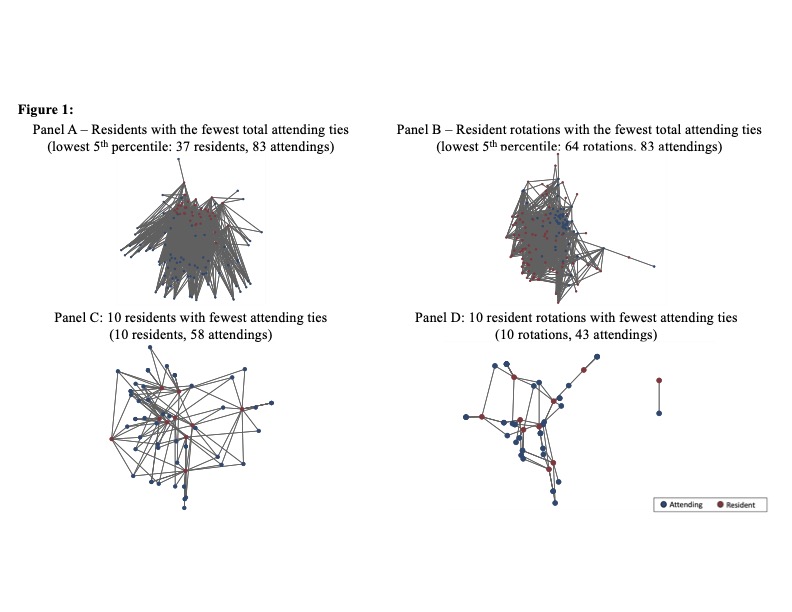
Results: During the study period, 526 residents completed 1013 unique rotations and 87 attendings provided instruction (Table 1). Social network analyses are shown in Table 2 and Figure 1. The average degree centrality for resident rotations (number of attendings supervising a resident per rotation) was 25.3 (standard deviation: ± 7.4) and did not vary significantly by program or PGY. The average degree centrality for attendings (number of residents supervised over study period) was 230.6 ± 116.5. Residents saw less than half of patients for the entire ED encounter (48.6%). Attendings rarely supervised the entire ED encounter for all patients seen with an individual resident (3453/25,655 observed resident rotation-attending dyads, 13.5%). The density of the network was 44% (20,064 observed resident-attending connections out of a possible 45,762).
Conclusion(s): Regardless of program or PGY, residents work with a large number of attendings during their PED rotation. This lack of longitudinal experiences is potentially exacerbated by residents seeing a minority of patients through their entire ED encounter.
.jpg)
