Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 3
650 - Telemedicine use trends in two different Medicaid-focused pediatric primary care clinics
Publication Number: 650.456

Nymisha Chilukuri, MD (she/her/hers)
Clinical Informatics Fellow
Stanford Medicine
San Francisco, California, United States
Presenting Author(s)
Background: With the COVID-19 pandemic, there was rapid implementation of telemedicine for Medicaid enrollees in pediatric primary care. Research is needed to understand the impact of this natural experiment on access to care and health inequities.
Objective: To compare telemedicine versus office visits during from March 2020-2021 including trends in use, reason for visit, and equity at two diverse Medicaid-focused pediatric primary care clinics.
Design/Methods: This retrospective cohort study included 17,142 visits among 8,375 patient 0-21 years from 3/15/20-3/15/21 at two Medicaid-focused pediatric primary care clinics (Site A and Site B). Data were extracted from the electronic health record. Primary outcomes were defined at the encounter level (telemedicine vs. office visit) and at the patient level (any telemedicine use vs. office visit use only). Secondary outcome was reason for visit (not mutually exclusive): well-child care (WCC), mental health care (MHC), acute care/follow-up (AC/FU). Demographic characteristics were child’s age, sex, race/ethnicity, preferred language, and payor. Descriptive statistics, univariable and multivariable mixed multilevel logistic regression were used to assess relationship between patient demographics and telemedicine use.
Results:
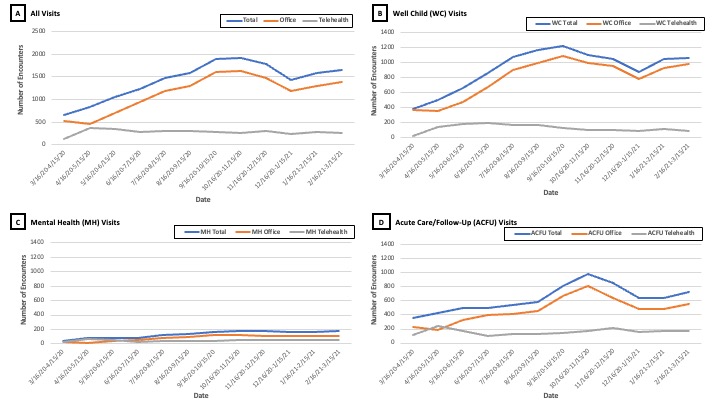
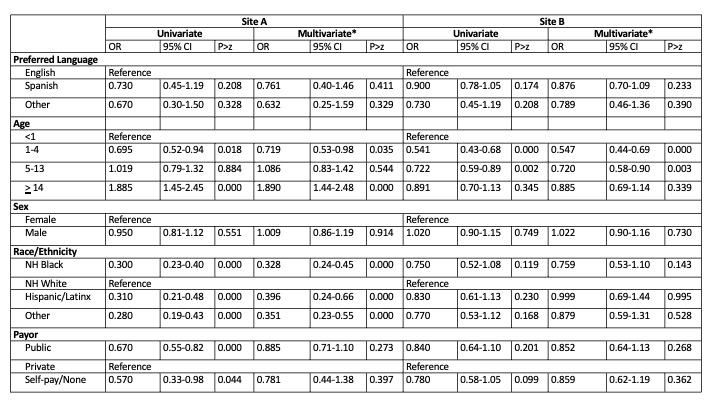
13% of all encounters at Site A (n=987) and 25% of encounters at Site B (n=2421) were conducted using telemedicine. At both sites, 13.8% of WCC (n=1515/10997), 36.2% of MHC (n=572/1581), and 25.0% of AC/FU (n=1893/7562) were telemedicine visits (Figure 1). After adjustment for covariates, at both sites, there were no statistically significant differences in odds of a patient having any telemedicine use by preferred language, sex, or payor (Table 1). At both sites, there were differences in odds of any telemedicine use by age. While at Site A, patients who identified as NH Black, Hispanic/Latinx or Other race/ethnicity had lower odds of telemedicine use in comparison to NH White, at Site B there was no difference in odds by race/ethnicity (Table 1).
Conclusion(s):
Telemedicine was successfully accessed by Medicaid-enrollees in different types of pediatric primary care (mental health, acute care/follow-up, and well child care). There was no difference in telemedicine use by preferred language and payor. However, differences existed by age at both sites and by race/ethnicity at one site. Future research should explore operational factors that improve telemedicine access for marginalized groups.