Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 9
581 - Do various neighborhood disadvantage indices equally predict child chronic health conditions?
Publication Number: 581.413
Deborah Winders Davis, PhD (she/her/hers)
Professor
University of Louisville School of Medicine
LOUISVILLE, Kentucky, United States
Presenting Author(s)
Background:
Social determinants of health are recognized as key drivers of health disparities. Understanding that race is a social construct, identifying the relationships between social opportunities resulting from racism and chronic health conditions is critical to removing barriers for optimal child outcomes. While measures of neighborhood disadvantage have emerged, little data are available on their validity for specific outcomes.
Objective:
The purpose of our study was to examine the distribution and associations between child chronic health conditions of four commonly used indices.
Design/Methods:
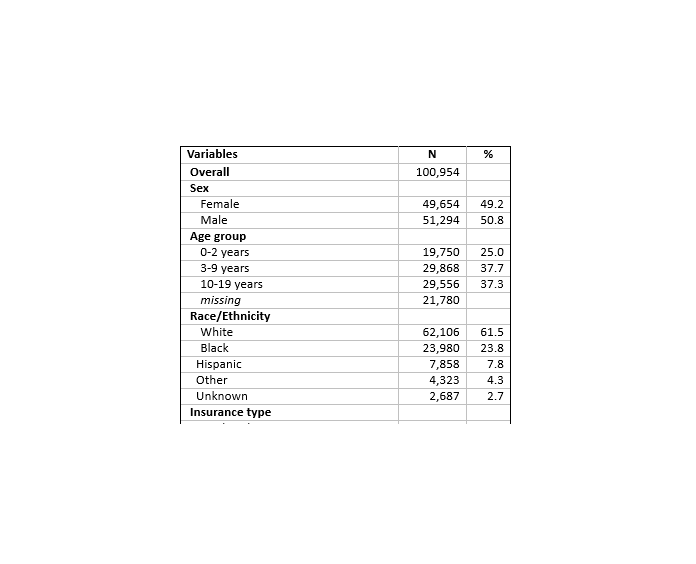
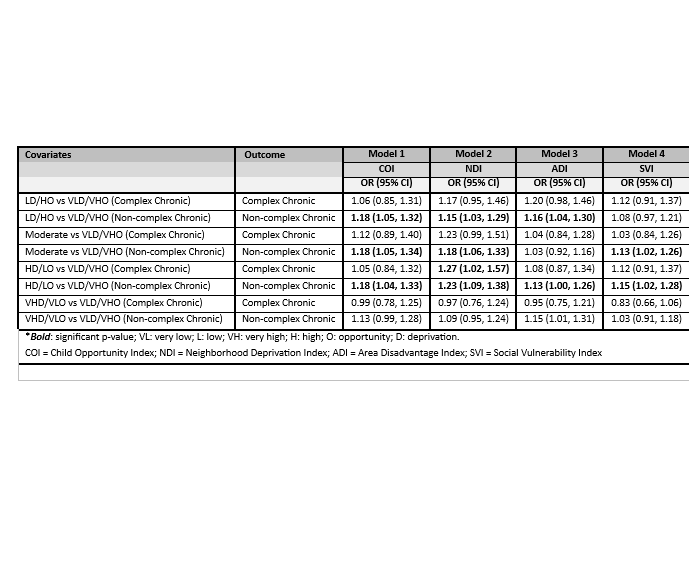
Outpatient visit data in 2019 (n=151,964) from a large children’s health system in an urban setting were used. Children with valid addresses living in the KY-IN Louisville Metropolitan Statistical Area (CBSA 31140; n=100,954) were included. Demographic data are described in Table 1. Measures of social disadvantage were the Child Opportunity Index (COI), Neighborhood Disadvantage Index (NDI), Area Deprivation Index (ADI), and Social Vulnerability Index (SVI). Child health outcomes included: no chronic disease, non-complex chronic disease, and complex chronic disease using the Pediatric Medical Complexity Algorithm (Simon, 2018). Separate multinomial logistic regression models for each measure were run and controlled for sex, race, age, and insurance type. For comparison, scores were converted to quintiles such that NDI, SVI, and ADI ranged from 1=least and 5=most deprivation and COI with 1=most and 5=least opportunity.
Results:
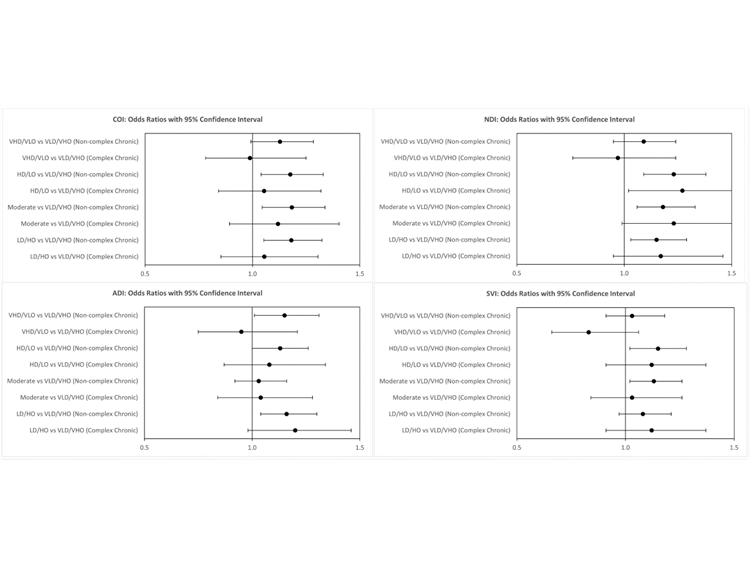
Variation in the odds ratios and their 95% confidence intervals for each measure are shown in Figure 1. Table 2 presents the adjusted odds ratios for the association between each quintile change of the four instruments to child health outcomes. These data suggest that COI and NDI are most predictive, and ADI is the least predictive of non-complex chronic disease.
Conclusion(s):
The four measures of disadvantage were not interchangeable. The indices have overlapping themes but are comprised of different factors. The COI findings seem counter-intuitive, but children with greater opportunity and access to care, may have a greater chance of receiving a diagnosis for a non-complex chronic condition, and consequently earlier intervention, than children with lesser opportunity. Importantly, our results support the need to carefully select a measure of neighborhood disadvantage or opportunity based on the study’s outcomes as different measures may yield different results.