Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 5
454 - SARS-CoV-2 Vaccine In Pregnancy: Assessment Of Maternal And Neonatal Immune Response During The First 9 Months After Delivery
Publication Number: 454.431

Alice Proto, MD (she/her/hers)
Attending physician
ASST Grande Ospedale Metropolitano Niguarda
Milano, Lombardia, Italy
Presenting Author(s)
Background: Risk of severe disease and mortality in pregnant women and newborns is greater if compared to non-pregnant adults in case of SARS-CoV-2 infection.
Objective: Our study’s aim is to assess the transfer of maternal antibodies in infants born to women vaccinated during pregnancy by measuring SARS-CoV-2 antibodies in maternal and infant blood samples at birth and during the first 9 months of life, to determine antibodies’ durability and to correlate antibody titer in the dyad.
Design/Methods: This is a prospective observational study on a cohort of pregnant women and their infants recruited on admission to delivery room from May to Nov 2021 at ASST GOM, Milan, Italy. All women received at least one dose of mRNA vaccine against SARS-CoV-2 during pregnancy at any trimester. Serological IgG antibodies anti-S1 RBD were evaluated through a quantitative chemiluminescent-assay.
Results:
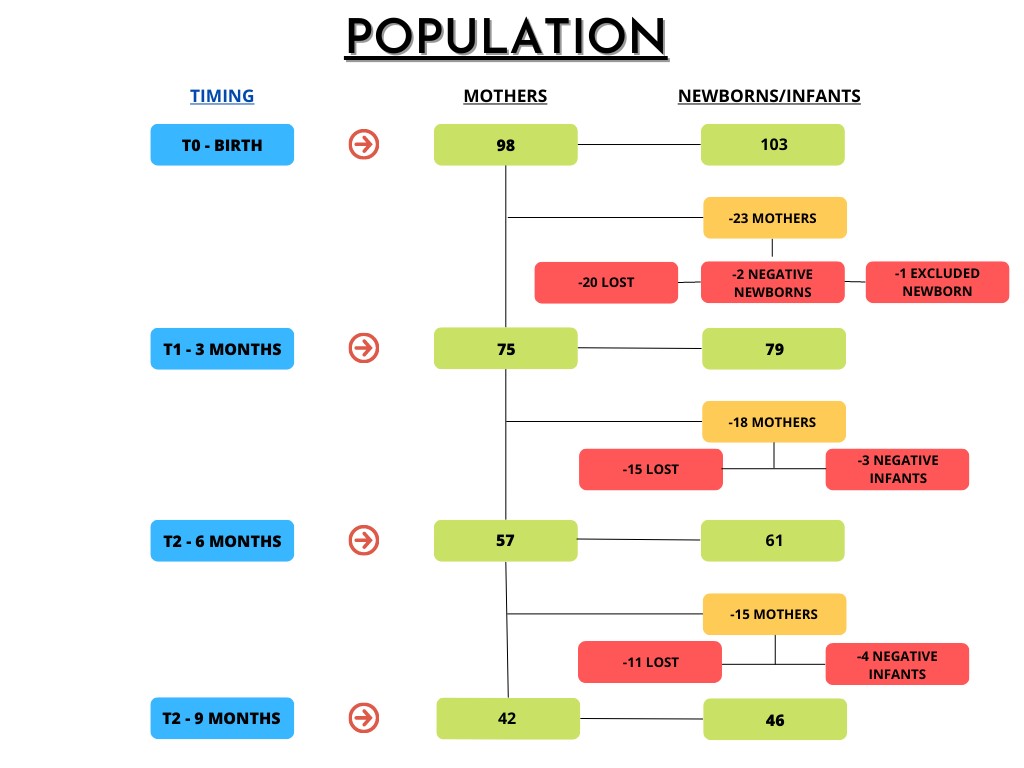
98 women and 103 babies were included in the analysis. Following delivery, maternal and neonatal peripheral blood samples were obtained at birth (T0), 3 months (T1), 6 months (T2) and 9 months (T3) after delivery.
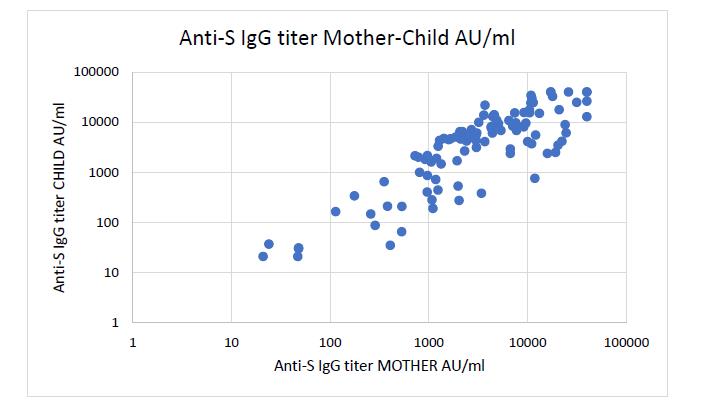
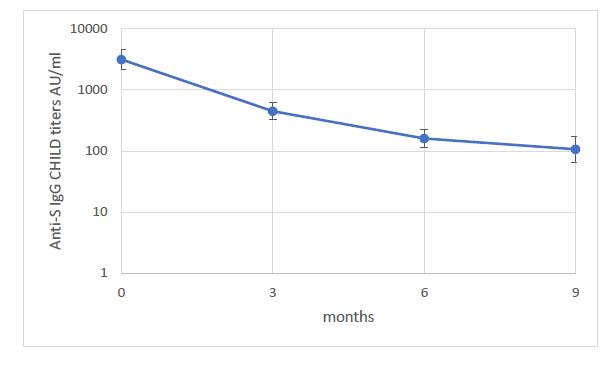
84% of women received BNT162b2 (Comirnaty) vaccine and 16% received COVID-19 Moderna mRNA-1273 (Spikevax) vaccine. Specific SARS-CoV-2 antibodies were found in both mothers and newborns at the time of delivery. We found a significant positive correlation between maternal serum levels of SARS-CoV-2 antibodies and neonatal serum levels at birth. Mothers vaccinated in the third trimester of pregnancy, and their respective newborns, have higher antibodies than the other two trimesters. The level of antibodies at birth decreases significantly over time, especially after 6 months. We observed a slower decline of antibodies titer in totally/partially breastfed babies if compared to formula fed babies.
Conclusion(s):
Our study demonstrates efficient transfer of SARS-CoV-2 IgG across the placenta from women vaccinated during pregnancy to their neonates, with a positive correlation between the maternal and neonatal sera antibody concentration. Antibody titer in children has a decreasing trend during the first months of life, but antibodies can be detected until 9 months after birth. Specific antibodies can be observed also in breastmilk, therefore breastfeeding must be encouraged for its potential protective role against infections, including SARS-CoV-2. SARS-CoV-2 vaccination during pregnancy must be strongly recommended as soon as possible at any time of gestation in order to maximize the protection of pregnant women and booster doses must be offered, especially during the third trimester, in order to protect the offspring.