Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 6
461 - Differential Diagnosis of a Spike in a Pulse Oximetry Warning System (POWS) Score for Sepsis in Very Low Birth Weight Infants
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 461
Publication Number: 461.432
Publication Number: 461.432
Claire Slevin, University of Virginia School of Medicine, Arlington, VA, United States; Sherry L. Kausch, University of Virginia School of Medicine, Charlottesville, VA, United States; Amanda Duncan, Washington University in St. Louis School of Medicine, St Louis, MO, United States; Zachary A. Vesoulis, Washington University School of Medicine, St. Louis, MO, United States; Douglas E. Lake, University of Virginia, Charlottesville, VA, United States; Karen Fairchild, University of Virginia School of Medicine, Charlottesville, VA, United States; Brynne A. Sullivan, University of Virginia School of Medicine, KESWICK, VA, United States

Claire Slevin, B.A.
Medical Student
University of Virginia School of Medicine
Arlington, Virginia, United States
Presenting Author(s)
Background: Late-onset sepsis (LOS) leads to high morbidity and mortality for very low birth weight (VLBW) infants. Cardiorespiratory changes occur in the preclinical phase of sepsis, prior to overt deterioration. We developed a pulse oximetry warning system (POWS) to analyze heart rate (HR) and oxygen saturation (SpO2) data and predict risk of imminent LOS diagnosis. While LOS is a major cause of cardiorespiratory instability, other infectious and non-infectious events can also lead to changes in HR and SpO2 patterns.
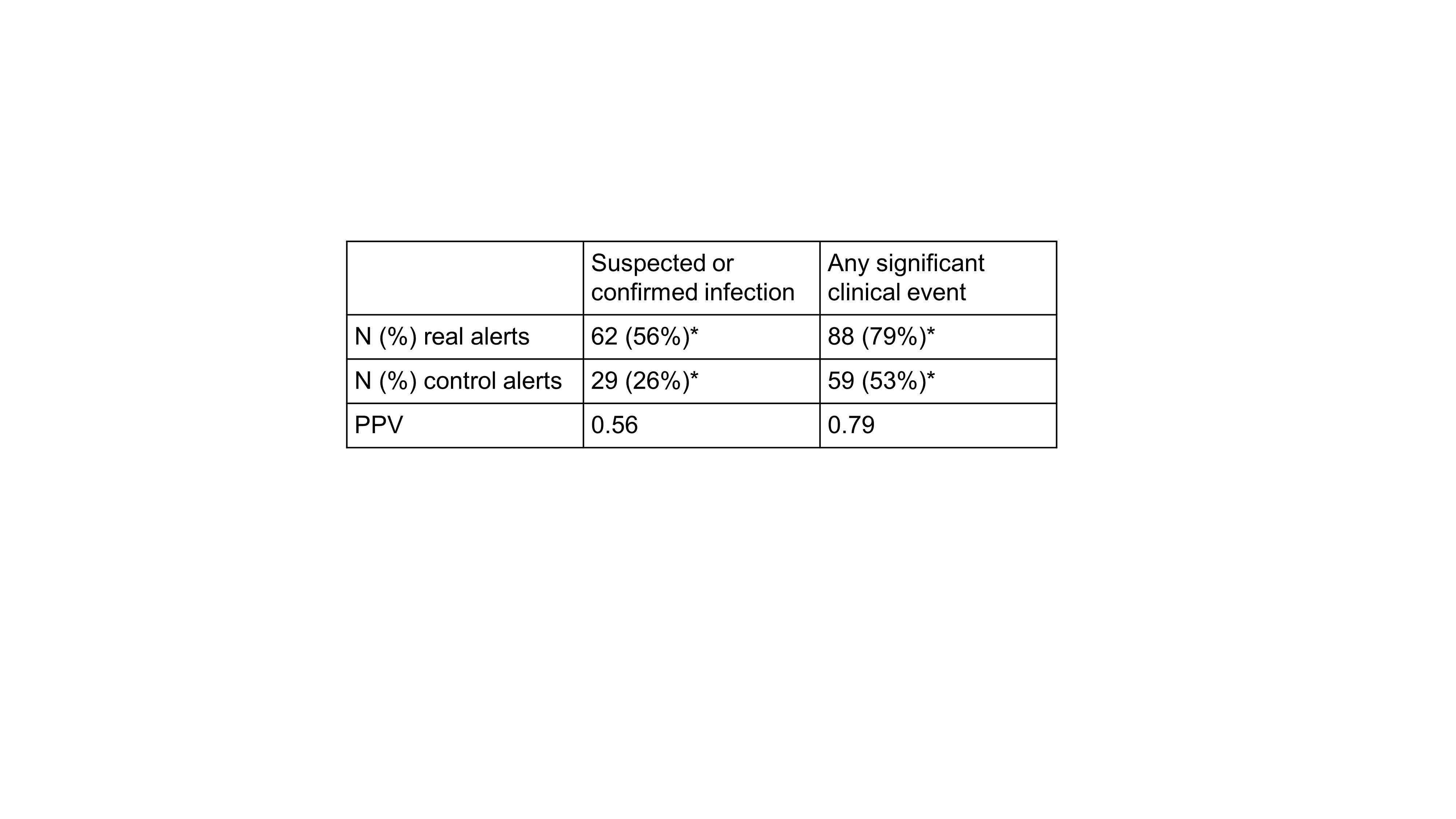
Objective: Determine the clinical correlations of a high POWS alert threshold and its positive predictive value (PPV) of for infectious vs. non-infectious clinical deterioration in VLBWs.
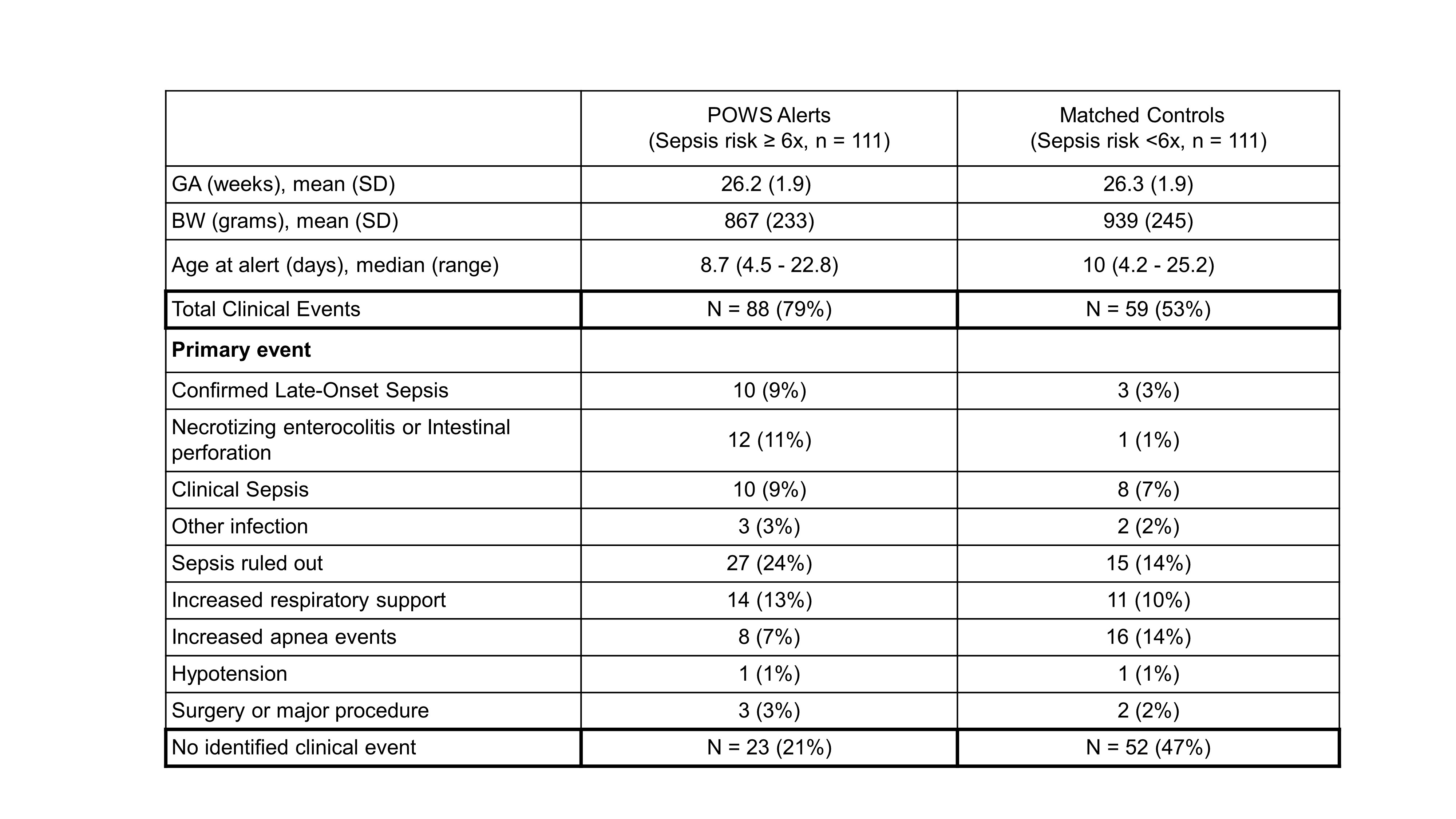
Design/Methods: In a two-NICU retrospective study, we randomly selected times when POWS increased above a risk score of 6 (POWS alert) with scores < 6 for 5 days prior. We selected an equal number of control times (POWS < 6), matched for gestational and chronologic age. We performed a blinded medical record review 3 days before and after the POWS or control alert times. We sought evidence of suspected or proven infection, including LOS (blood culture positive beyond 72h of age), clinical sepsis, sepsis ruled out, other infection, and necrotizing enterocolitis. Additionally, we sought evidence of non-infectious events, including major respiratory deterioration (significant increase in support and/or apnea) and surgery. We calculated the relative frequencies and estimated the PPV of a POWS alert for infectious and any clinically significant events within 3 days.
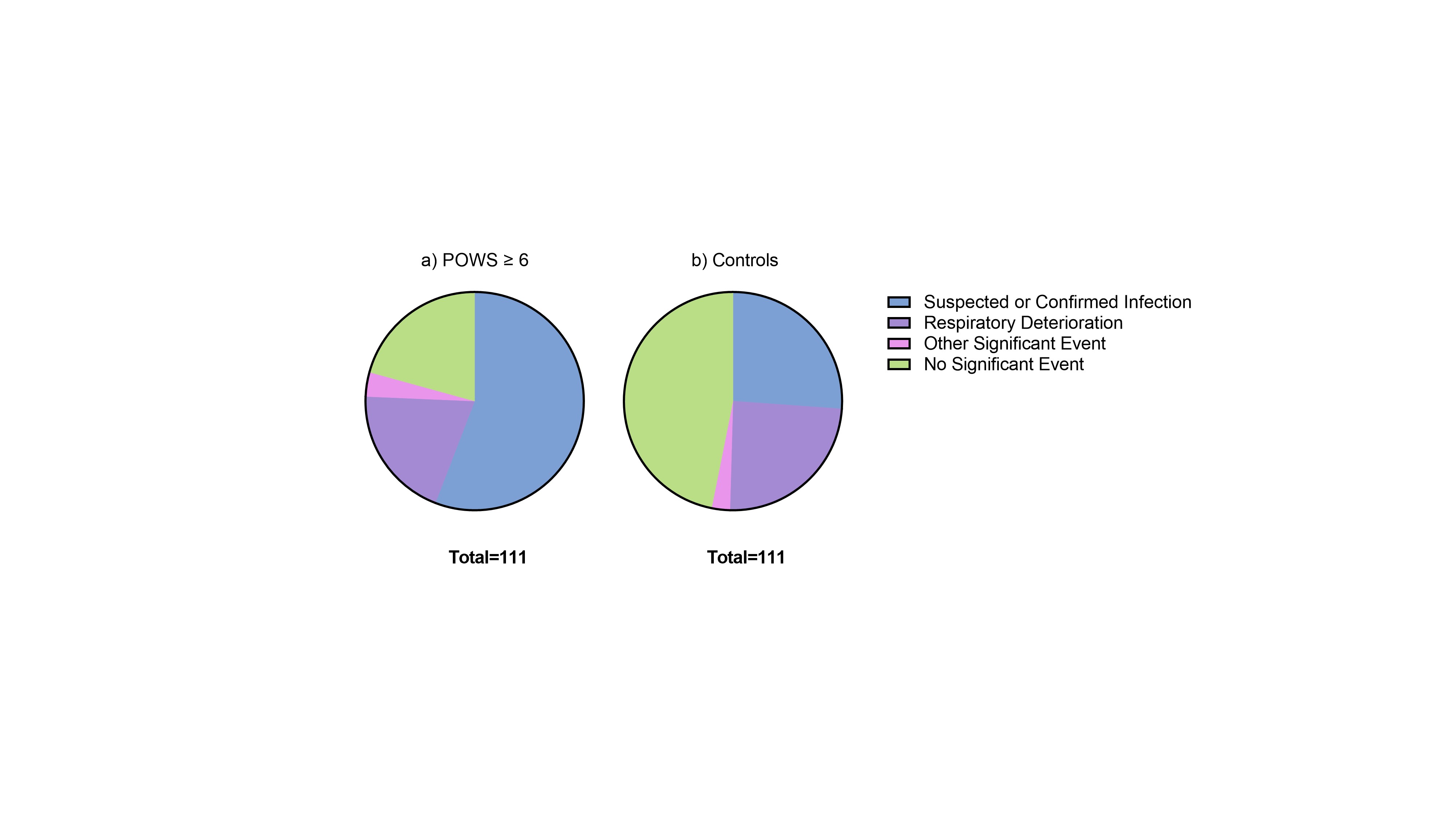
Results: We analyzed 111 POWS alerts and 111 control times from 192 VLBW infants (Table 1). Significant clinical events occurred near 88 (79%) POWS alert times compared to 59 (53%) control times (Fig. 1). POWS alert times were more likely to occur near clinically significant events including suspected or proven infection than control times (Table 2). The high POWS alert had a PPV of 0.56 for infectious conditions and 0.79 for any clinically significant event. Respiratory deterioration occurred near a similar proportion of POWS alert and control times (20% vs 24%). For POWS alerts associated with LOS, 70% had an alert prior to the time of the positive blood culture (mean 35h before).
Conclusion(s): In VLBW infants at 2 NICUs, a high POWS cardiorespiratory sepsis risk score had a high PPV for suspected or confirmed infection and higher PPV when respiratory deterioration events unrelated to infection were included. POWS monitoring could be useful as an early warning system to alert clinicians when a VLBW infant has a high risk of cardiorespiratory deterioration.