Infectious Diseases
Infectious Diseases 5
438 - Non-severe Multi-system Inflammatory Syndrome-like Illness: Were We Treating this as Incomplete Kawasaki Disease Prior to the Pandemic?
Publication Number: 438.419

Lucie K. Fan, BS (she/her/hers)
Medical Student
Lucie Fan
Chamblee, Georgia, United States
Presenting Author(s)
Background:
The clinical features of multisystem inflammatory syndrome in children (MIS-C) overlap with Kawasaki Disease (KD). A prior clinical scoring system differentiated children with MIS-C from those with pre-pandemic complete KD (cKD) or incomplete KD (iKD) with coronary abnormalities. We retrospectively assessed its performance in differentiating children with non-severe MIS-C from those with iKD without coronary involvement.
Objective: The objective of our retrospective observational study was to compare the clinical presentations and laboratory parameters between children diagnosed with incomplete KD (iKD) pre-SARS-CoV-2 pandemic with children with MIS-C whose management did not require intensive care and who had normal coronary arteries. We hypothesized that there was a considerable clinical and laboratory overlap between patients previously treated for iKD and patients treated for MIS-C.
Design/Methods:
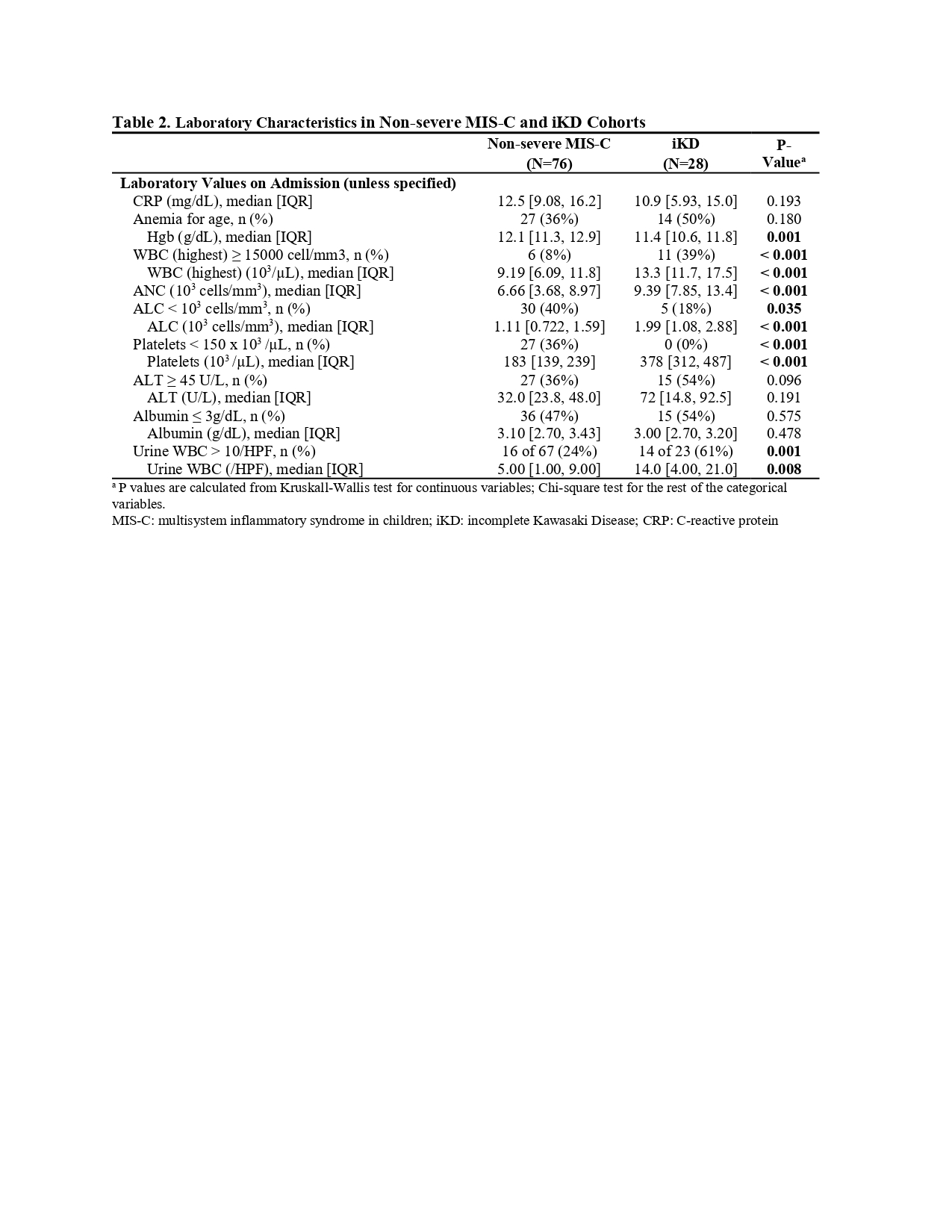
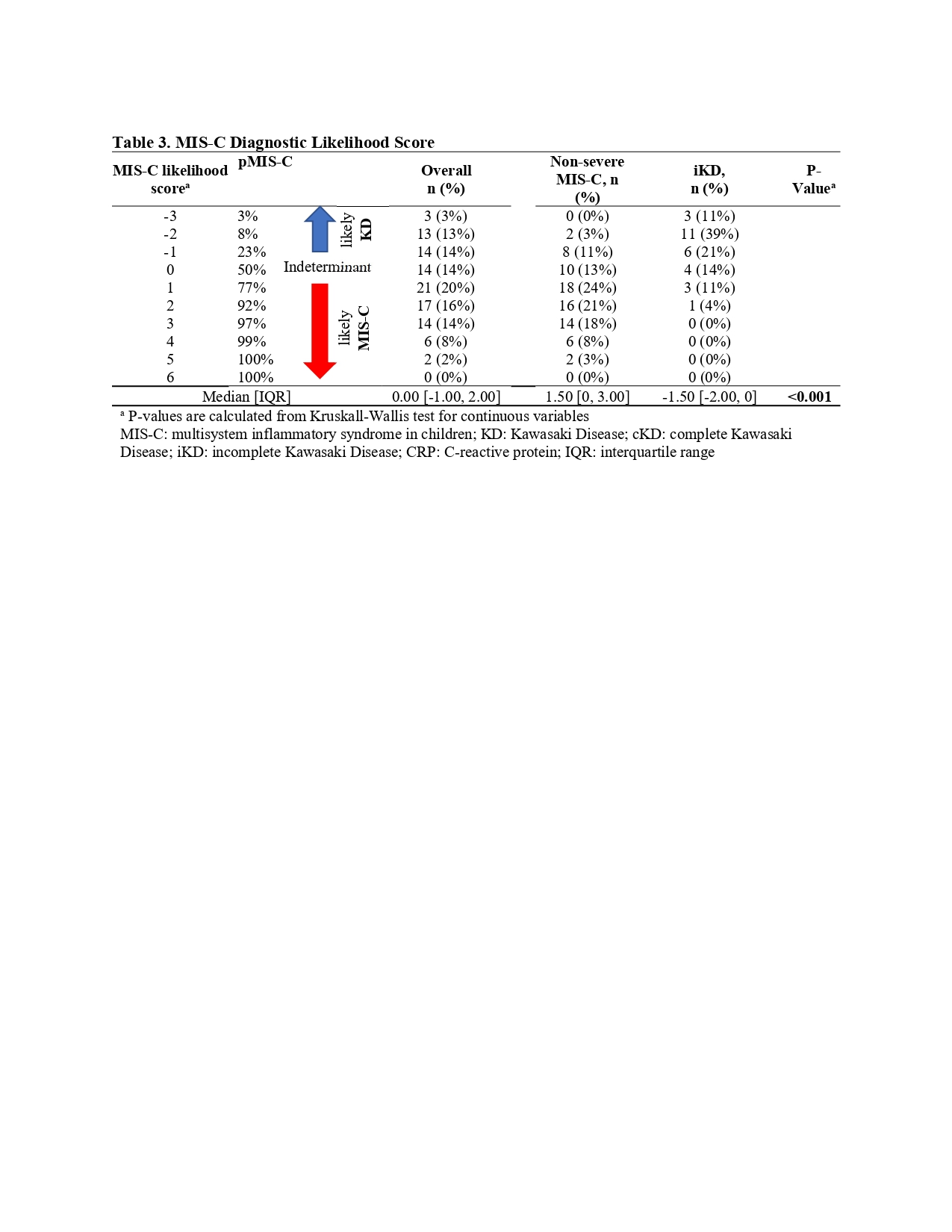
We classified children with iKD (1/2018-1/2019) and non-severe MIS-C (3/2020-2/2021) as those who met criteria from the American Heart Association and CDC and were treated for their respective diagnoses at our facility, excluding those with intensive care and coronary abnormalities in both cohorts. We applied the scoring system [features favoring MIS-C: thrombocytopenia, abdominal pain, headache, pericardial effusion, C-reactive protein (CRP) >10 mg/dL] and estimated the percent of children with iKD who could have met the inflammation and organ system criteria of the CDC MIS-C classification, had they presented during 2020-2021.
Results: Ninety-three percent of 28 children with iKD met the MIS-C surveillance definition. The non-severe MIS-C cohort (n = 76) were older (8 vs. 4 years), and more likely to have neurological symptoms versus those with iKD (54% vs. 14%). Upon admission, patients with non-severe MIS-C had higher rates of thrombocytopenia and lymphopenia (p = 0.035), while those with iKD had leukocytosis. Those with iKD had higher rates of pyuria (61% vs. 24%; p < 0.001 for all comparisons unless specified). The scoring system identified concordance with 74% and 71% of the children from the non-severe MIS-C and iKD cohort, respectively, meeting their clinical diagnosis.
Conclusion(s): Though there is considerable overlap, findings on a basic blood count were helpful to distinguish those with non-severe MIS-C vs iKD..jpg)