Medical Education: Resident
Medical Education 15: Resident 6
509 - Improving Safe Sleep Education for Residents
Publication Number: 509.423

Hannah Levine, MD (she/her/hers)
Resident
The Children's Hospital at Montefiore
Bronx, New York, United States
Presenting Author(s)
Background: Sudden Infant Death Syndrome (SIDS) is one of the leading causes of death in infants. In the 1990s, the incidence of mortality from SIDS decreased sharply, since then rates are increasing. The 2017 New York State Child Fatality report states infant deaths represent the largest number of child fatalities, and unsafe sleep habits continue to be the most common cause. Since 2015, the Bronx ranks in the top 3 for infant deaths in New York.
Objective: Our objective was to use an educational intervention to improve pediatric residents’ frequency and comfort providing safe sleep counseling during newborn to 6-month health care maintenance (HCM) visits in two resident pediatric clinics in the Bronx.
Design/Methods:
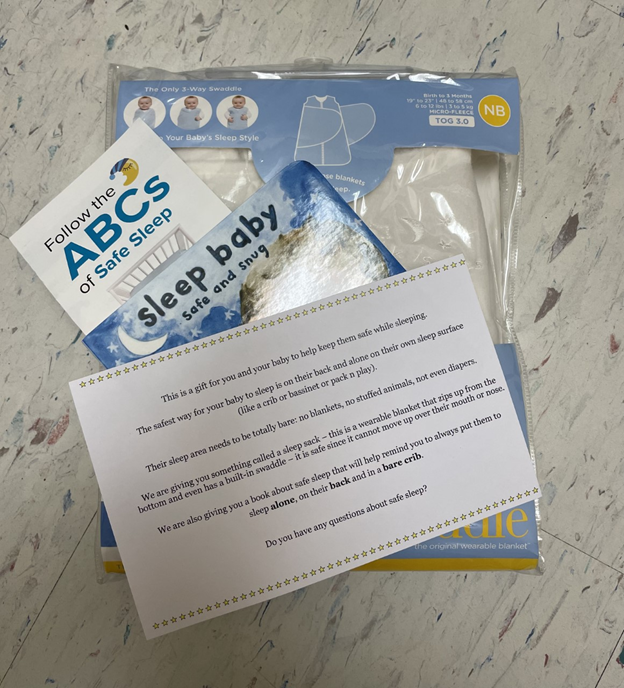
This was a pre-post survey study examining the impact of our safe sleep intervention on pediatric residents at the Children’s Hospital at Montefiore in the Bronx, NY. The intervention was targeted in two main pediatric resident clinics. The clinics provide primary care to the Bronx community, which is composed of a diverse, lower socioeconomic status population. Our intervention included a safe sleep didactic and a safe sleep bundle (safe sleep book, pamphlet, sleep sack and patient script). The bundle was created using funding from an American Academy of Pediatrics’ (AAP) Community Access to Child Health grant. Residents were given the pre-survey prior to the intervention, and the post-survey was given 2 months later. Outcomes were measured using the Wilcoxon signed-rank test. Our results indicate post-intervention, there was a statistically significant difference in both residents' frequency providing and comfort with AAP safe sleep recommendations. This study demonstrates that using targeted educational tools is impactful in reinforcing safe sleep counseling. We are hopeful this can translate into safer sleep practices in the Bronx, NY and beyond.
Results: Of 50 residents who completed the survey, 19 were included in the study for having pre- and post-survey matches. Frequency of safe sleep (FSS) counseling was measured with a FSS number (Never = 1, Rarely = 2, Sometimes = 3, Always = 4) and averaged across age visits (newborn, 2-month, 4-month and 6-month). Using the Wilcoxon signed-rank test, we compared the mean FSS number between pre- (3.39) and post- (3.63) survey results. There was a statistically significant difference in frequency of safe sleep counseling given over newborn to 6-month HCM visits (p < 0.05). As a secondary measure, resident comfort with the AAP Safe Sleep recommendations also showed a statistically significant difference (p < 0.05) after our intervention.
Conclusion(s):