Injury Prevention
Injury Prevention 2
313 - A Novel Approach to Increasing Infant Safe Sleep Practices Through the Pediatric Emergency Department in The East Baltimore Community
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 313
Publication Number: 313.42
Publication Number: 313.42
Kala Frye Bourque, Children's National Health System, Silver Spring, MD, United States; Leticia M. Ryan, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Mary Beth Howard, The Johns Hopkins School of Medicine, Baltimore, MD, United States; Eileen M. McDonald, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; Isabella Lelis, Johns Hopkins Children's Center, Scarsdale, NY, United States; Brian H. Min, Johns Hopkins University School of Medicine, Salisbury, MD, United States; Hannah Hardeo, Johns Hopkins Children's Center, Baltimore, MD, United States

Kala Frye Bourque, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's National Health System
Silver Spring, Maryland, United States
Presenting Author(s)
Background: Baltimore City has a rate of infant co-sleeping and sleep-related deaths 1.3 times higher than Maryland and 1.5 times higher than the U.S. The pediatric emergency department (PED) is a prime location to reach at-risk families to increase infant safe sleep practices, as it serves those with limited or pandemic-related disruptions to primary care. However, practical challenges exist to provide supplies through the PED including lack of space and families transporting supplies home.
Objective: To pilot a PED-based infant safe sleep promotion program distributing portable cribs and sleep sacks by home delivery to families with infants who report unsafe sleeping practices.
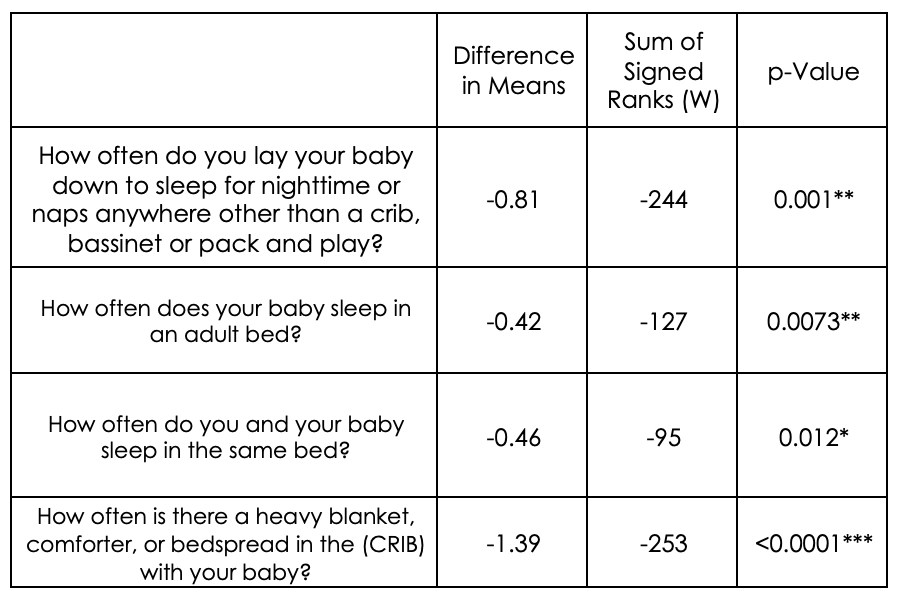
Design/Methods: A convenience sample of families with infants < 6 months in a PED in Baltimore, MD were approached and enrolled if the parent expressed a need for a portable crib and/or sleep sack. Participating families completed a 10 question pre-intervention survey about current infant sleep practices. Research staff ordered a portable crib and sleep sack to be shipped directly through Amazon to the family and tracked delivery confirmation. One month after enrollment, families completed a telephone survey about current infant sleep practices and perceptions about the program. Descriptive statistics summarize the data on feasibility, acceptability, and effectiveness. To assess infant sleep practice changes, nominal values on a scale of 0-4 were applied to the ordinal categorical variables (Never= 0, Seldom= 1, About Half= 2, Usually= 3, Always= 4). A Wilcoxon Signed Rank Test at the 0.05 level of confidence was then used to assess overall behavior risk changes.
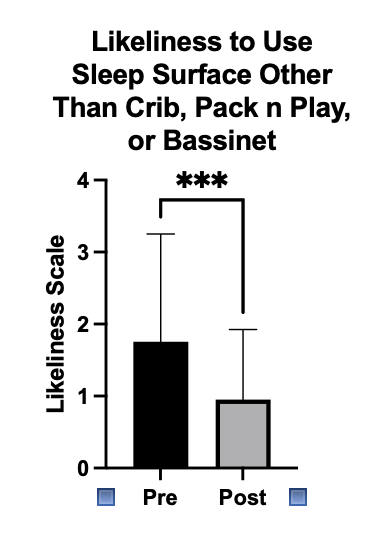
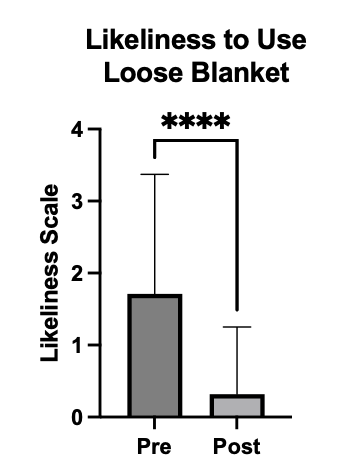
Results: Of 64 infants screened in the PED, 50 (78%) were enrolled. Mean age was 2.8 months (SD 0.22) and the majority (46, 92%) received their Amazon delivery on first attempt. Most (42, 84%) completed post-surveys; 38 (91%) reported the supplies were easy to use. All expressed positive sentiment about the program. A comparison of pre to post on a scale of 0- 4 found a significant decrease of use of unsafe sleep surfaces (-0.81, p=0.0001); use of an adult bed for sleeping (-0.42, p = 0.0073), co-sleeping with an adult (-0.46, p = 0.0012), and use of loose blankets (-1.39, p = < 0.0001).
Conclusion(s): Our data support the feasibility, acceptability, and effectiveness of this pilot program. Provision of portable cribs and sleep sacks via home delivery to PED families with infants at risk of sleep- related death was feasible and reduced unsafe sleep practices. Next steps include replication of this pilot study on a larger scale.