Infectious Diseases
Infectious Diseases 4
417 - Assessment for Differences in Antibiotic Use for Acute Otitis Media in Pediatric Urgent Care
Publication Number: 417.418
.jpg)
Kevin Lloyd, MD (he/him/his)
Infectious Diseases Fellow
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Acute otitis media (AOM) is one of the most diagnosed conditions in pediatric urgent care and the most common indication for antibiotics in children. Observation without antibiotics for nonsevere AOM in children >6 months is recommended as a safe management option but is underutilized. Racial differences related to antibiotic prescribing exist in multiple care settings, with White children more likely to receive an unnecessary antibiotic for a viral infection than non-White children.
Objective:
To determine if there are sociodemographic differences between children >6 months of age who receive an immediate antibiotic prescription in the urgent care setting for nonsevere AOM compared with those who do not.
Design/Methods:
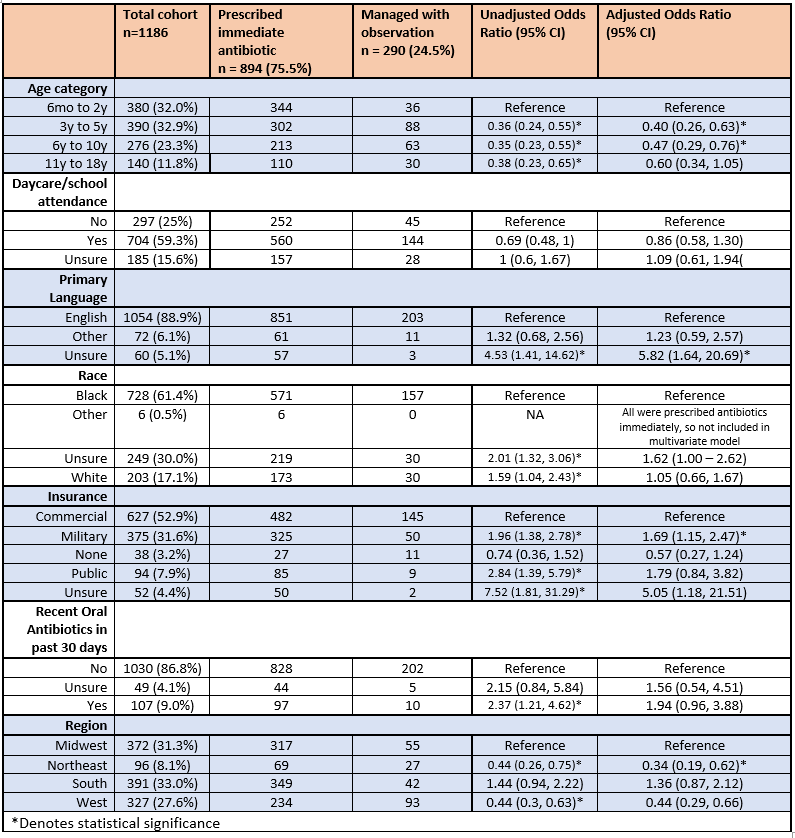
This was a secondary analysis of survey data collected from pediatric urgent care encounters as part of a multi-institutional QI project occurring from June 2019 to December 2020. We included patients 6 months to 18 years evaluated at a participating free-standing pediatric urgent care and diagnosed with nonsevere AOM as defined by AAP Clinical Practice Guidelines. Primary exposures were race (categorized as Black, White, other, unsure), primary language (English, other, unsure), and insurance status (commercial, public, military, none, unsure). Univariate analysis of each variable of interest was performed on the probability of receiving an antibiotic using chi-squared tests. A priori variables of interest (race, primary language, insurance status, daycare/school attendance) and any variables associated with antibiotic administration at a p-value of < 0.20 were included in a logistic regression analysis.
Results:
1,186 nonsevere AOM encounters were included. Mean age was 4.99 years (stdev 3.99 years); 728 (6.4%) were Black, 203 (17.1%) were White; 72 (6.1%) reported a language other than English; 627 (52.9%) had commercial insurance, 375 (31.6%) had military insurance, and 94 (7.9%) had public insurance. 894 patients (75.5%) were immediately prescribed antibiotics. In multivariate analysis, patients with military insurance were significantly more likely to be prescribed antibiotics (aOR 1.69; 95% CI:1.15, 2.47). Neither race nor primary language was significantly associated with antibiotic prescription in multivariate analysis. (Table 1)
Conclusion(s):
Among a population of children >6 months presenting to pediatric urgent care with nonsevere AOM, 75% of children were immediately prescribed antibiotics. Children with military insurance had a higher likelihood of receiving antibiotics. No association between antibiotic prescription receipt and race or primary language was observed.