Medical Education: Resident
Medical Education 15: Resident 6
505 - Communicating and Connecting: Developing a Curriculum on Prenatal Counseling for Residents
Publication Number: 505.423

Michelle J. Bartlett, MD, MS (she/her/hers)
Resident Physician
University of Washington School of Medicine
SEATTLE, Washington, United States
Presenting Author(s)
Background:
Late preterm infants comprise 75% of premature births and are born physiologically immature with a greater risk of health complications than term infants. Residents in pediatrics (peds), obstetrics (OB) and family medicine (FM), are often called upon to provide prenatal counseling for families expecting late preterm infants. Training opportunities typically focus on the very preterm infants and there is a lack of known prenatal counseling curricula that focus on late preterm counseling skills.
Objective: Our aim was to perform a ‘needs based’ assessment to develop a curriculum to teach residents, of various specialties, skills in late preterm prenatal counseling.
Design/Methods: Participants were recruited from the University of Washington peds, OB, and FM residency programs to complete an anonymous survey on baseline confidence in elements of a late preterm prenatal counseling visit based on the previously validated Antenatal Counseling Milestones Scale (ACoMS).
Results:
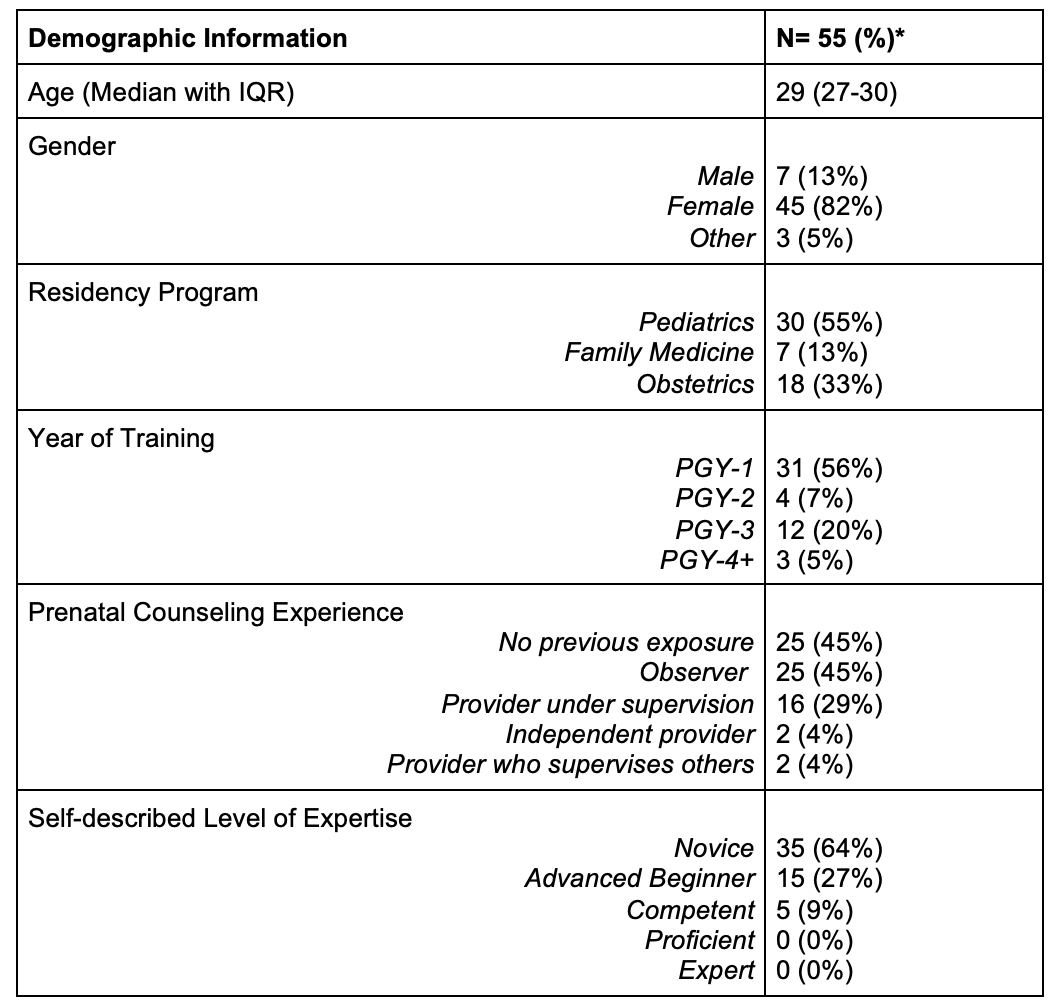
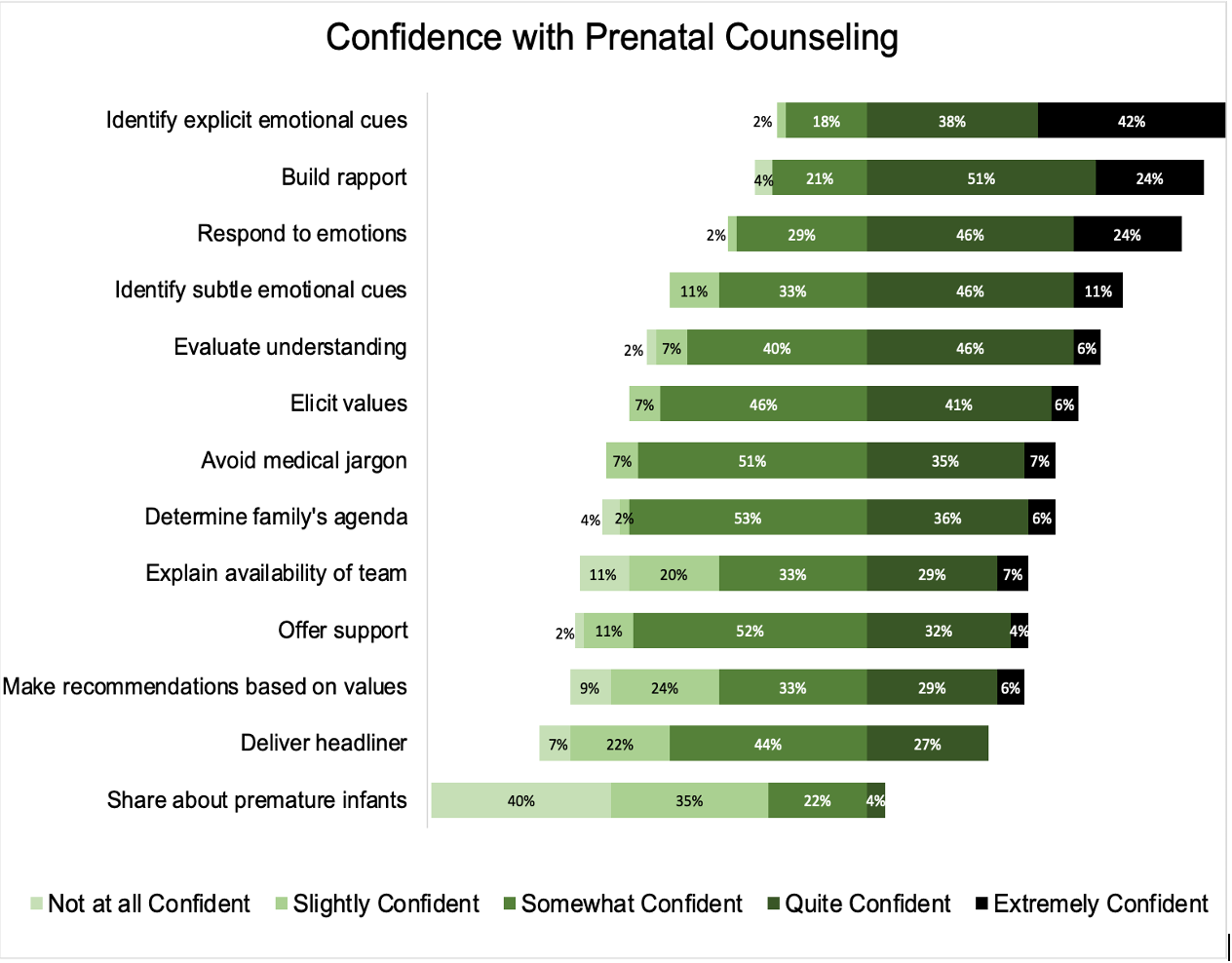
55 surveys were completed. Table 1 shows demographic information about participants. Most participants were in their first year of training and 90% had little to no previous experience with prenatal counseling (Table 1). A total of 8(44%) OB residents, 1(14%) FM resident, and 4(13%) peds residents had performed at least 1 prior prenatal consult. Baseline comfort levels with the principal elements ranged from “Not at all confident” to “Extremely confident”. Fifty-four percent of seniors (⪰PGY-2) felt quite or extremely confident across all elements compared to only 40% of interns. Participants felt most confident in their ability to build rapport, identify emotional cues, and respond to those emotions and least confident about sharing medical information about premature babies (Figure 1).
Conclusion(s): Most residents had limited exposure to prenatal counseling for late preterm infants and were least confident in sharing information about late preterm babies and making recommendations based on family’s values. Areas in which residents felt most confident, such as building rapport and responding to emotional cues, are communication skills that are not mutually exclusive to the prenatal consult. The results of this needs assessment will help inform the development of an essential late preterm prenatal counseling curriculum integrated with the ACoMS assessment for use by peds, OB, and FM residencies.