Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 2
626 - A Comparison of Teleburn to In-person Consultations of Pediatric Patients in a Children’s Emergency Department
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 626
Publication Number: 626.455
Publication Number: 626.455
Claci Ayers, Vanderbilt University School of Medicine, Nashville, TN, United States; Hannah Byrd, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Rebecca Kidd, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Barbara Solomon, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Stephen Gondek, Vanderbilt University Medical Center, Nashville, TN, United States; Anne Wagner, Vanderbilt University School of Medicine, Nashville, TN, United States; Ronnie Mubang, Vanderbilt University School of Medicine, Nashville, TN, United States

Claci Ayers, MD
Pediatric Emergency Medicine Fellow
Vanderbilt University School of Medicine
Nashville, Tennessee, United States
Presenting Author(s)
Background: Pediatric Burn Care is an essential component to pediatric emergency care. Regional Burn Centers provide burn care but unfortunately there are disparities in access to regional burn centers for pediatric patients. Teleburn is a tool that enables providers without a certified burn center to provide photos of a burn to experts and receive recommendations on burn care.
Objective: The purpose of this study is to evaluate the effectiveness of a Teleburn system to the gold standard in-person consultation in regards to burn infection rate, clinic follow up rate, post-burn admission rate, and 72-hour bounce back rate.
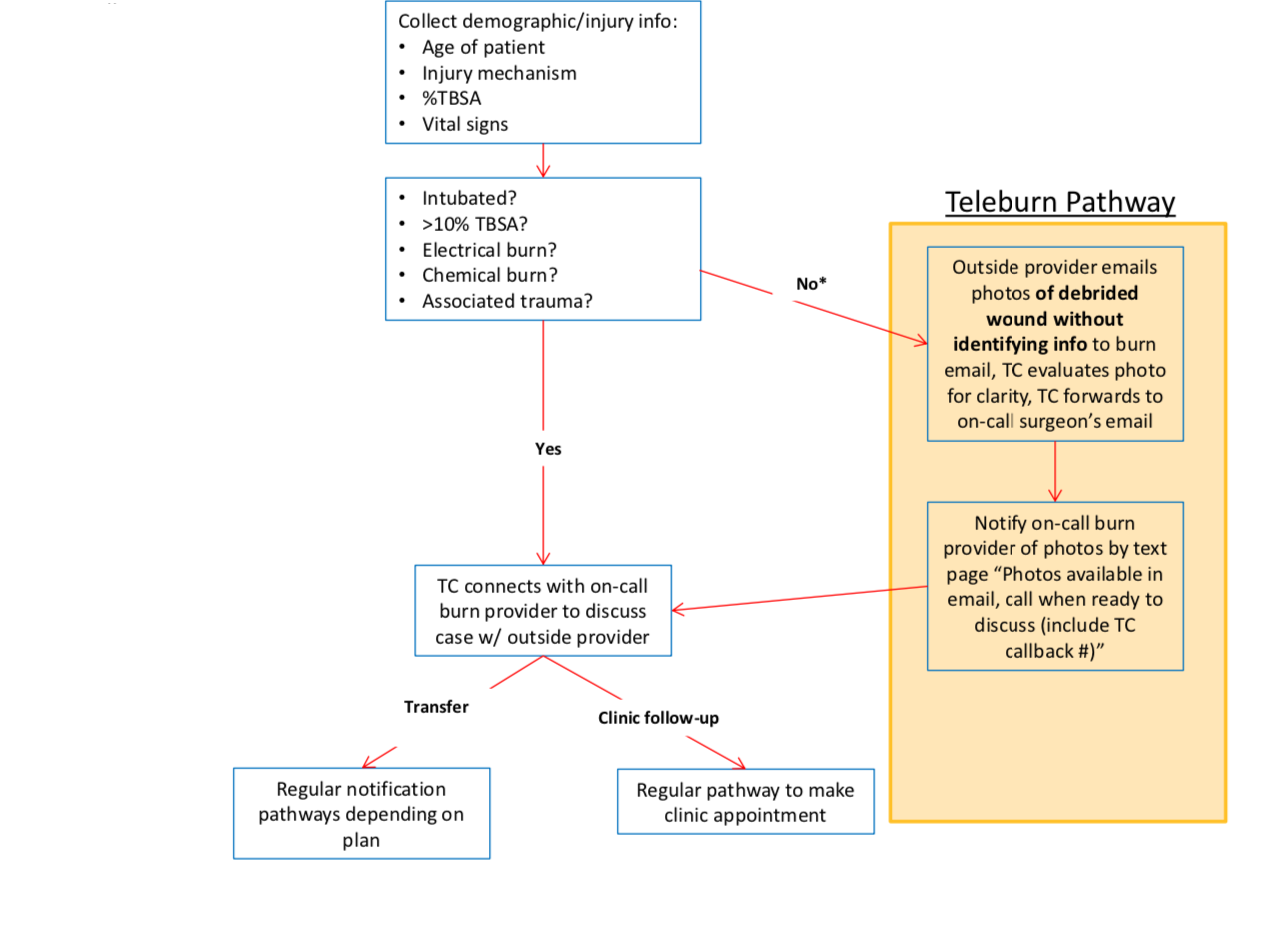
Design/Methods: Data was collected from December 2019-March 2022 through the electronic medical record. A total of 416 patient encounters that met criteria were analyzed. The criteria for a Teleburn encounter are displayed in Fig. 1 and this was the criteria applied to the in-person burn consults. A non-inferiority study was designed comparing proportional outcomes of telemedicine burn initial visits to emergency department visits in regard to burn infection rate, clinic follow up rate, post-burn admission rate, and 72-hour bounce back rate. The data were compared with a difference of greater than 10% being considered inferior.
Results: Amongst the patient encounters 45.6% were female and ages ranged from 7 weeksto 19 years. Most common burn type was scald at 47.5%, with thermal being second at 43.7%. No differences were identified in rates of readmission - 1.67% difference (95% CI -27%< x< 23.8%) and return within 72 hours – 0.7% difference (-18.4%< x< 19.7%). Teleburn patients were 12.6% less likely to follow up (2.7%< x< 22.40%). Only one infection was identified, which is insufficient to conclude non-inferiority in terms of infection events.
Conclusion(s): While convenient, Teleburn consult could not be demonstrated to be non-inferior to in-person consultation. No differences in infection rates were identified, and difference in readmission and return were clinically insignificant. Efforts to improve follow-up may prove successful in raising the standard to that of in person visits given the large geographic areas covered by most regional burn centers.This research advocates for more enhancement of Teleburn consult systems for pediatric acute minor burns and presents easily surmountable limitations. This study demonstrates that telemedicine may be effective and feasible to regional burn centers if follow up can be improved.