Emergency Medicine: All Areas
Emergency Medicine 14
376 - Comparison of a Rapid Multiplex Gastrointestinal Panel with Standard Laboratory Testing in the Management of Children with Hematochezia in a Pediatric Emergency Department: Randomized Controlled Trial
Publication Number: 376.405

Stephen Freedman, MDCM, MSc (he/him/his)
Professor of Pediatrics and Emergency Medicine
University of Calgary
Calgary, Alberta, Canada
Presenting Author(s)
Background: Acute bloody diarrhea is a medical emergency and as the etiology is often unknown, blood tests are frequently performed. However, recent advances in diagnostic microbiology allow for the identification of a broad range of enteropathogens within hours and such knowledge could inform care and reduce the need to additional testing.
Objective: To determine if a rapid enteric diagnostic platform reduces blood testing in children with hematochezia.
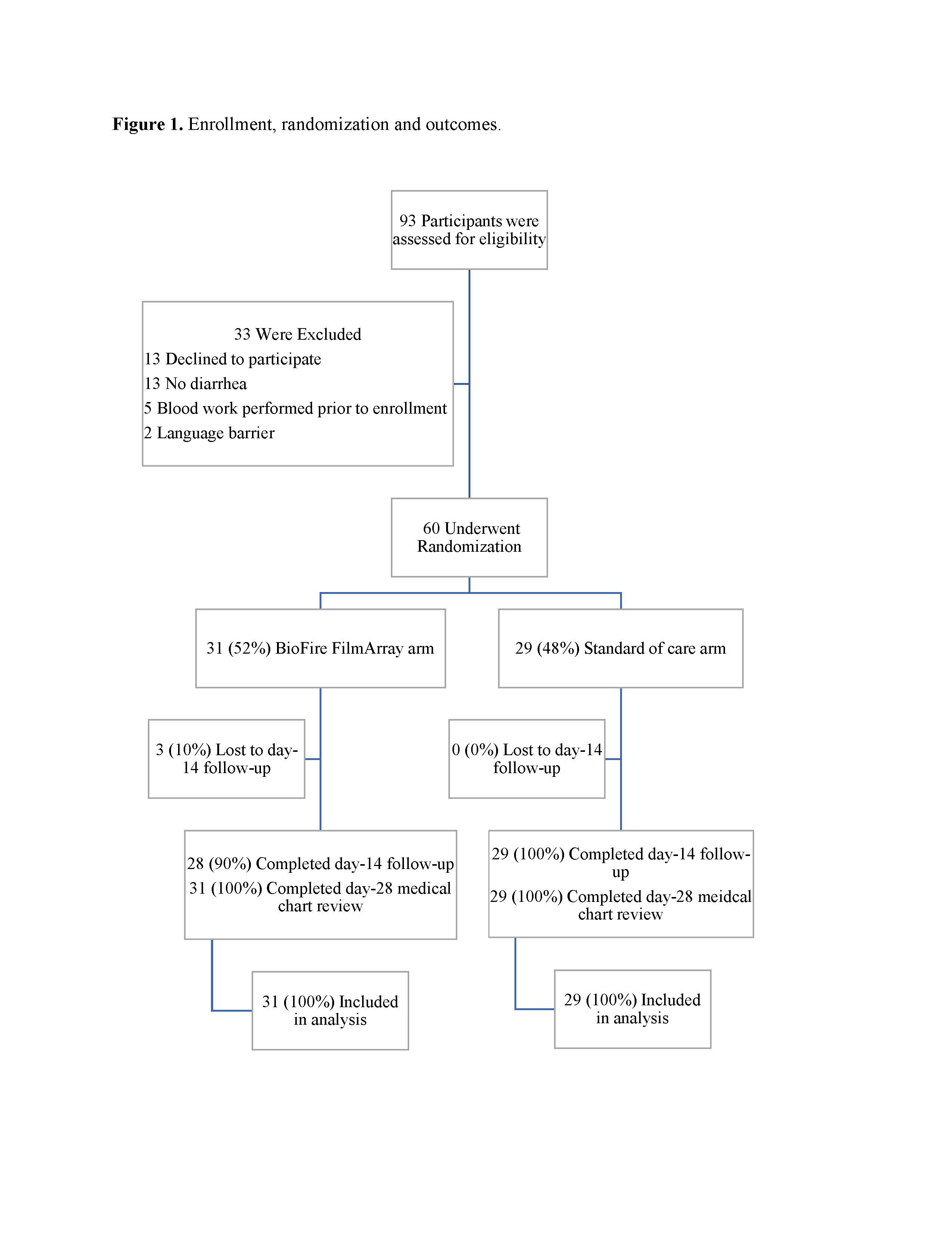
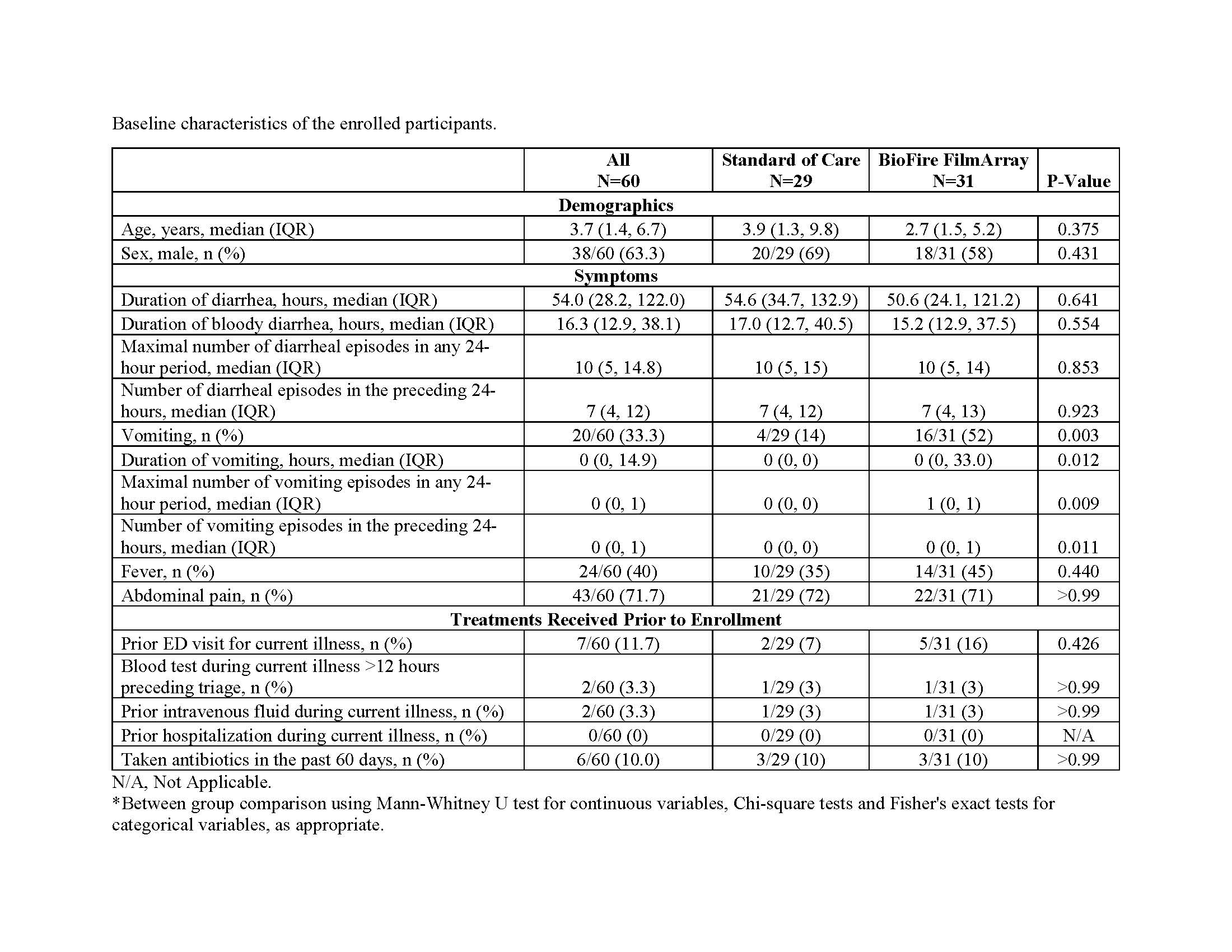
Design/Methods: We conducted a single-center, randomized, unblinded trial in a tertiary-care pediatric ED. Participants were randomized to have stool tested using our laboratory’s routine bacterial identification approach (i.e. culture which switched to a limited batched molecular panel partway through the study) or to use of the BioFire FilmArray Gastrointestinal Panel which identifies 22 pathogens with a 1-hour instrument turnaround time. All participants had rectal swabs performed if stool was not immediately available. Eligible participants were aged 6 months to < 18.0 years and presented for care due to bloody diarrhea. The BioFire test result was provided to the responsible physician. The primary outcome was the performance of any blood test within 72 hours of randomization.
Results:
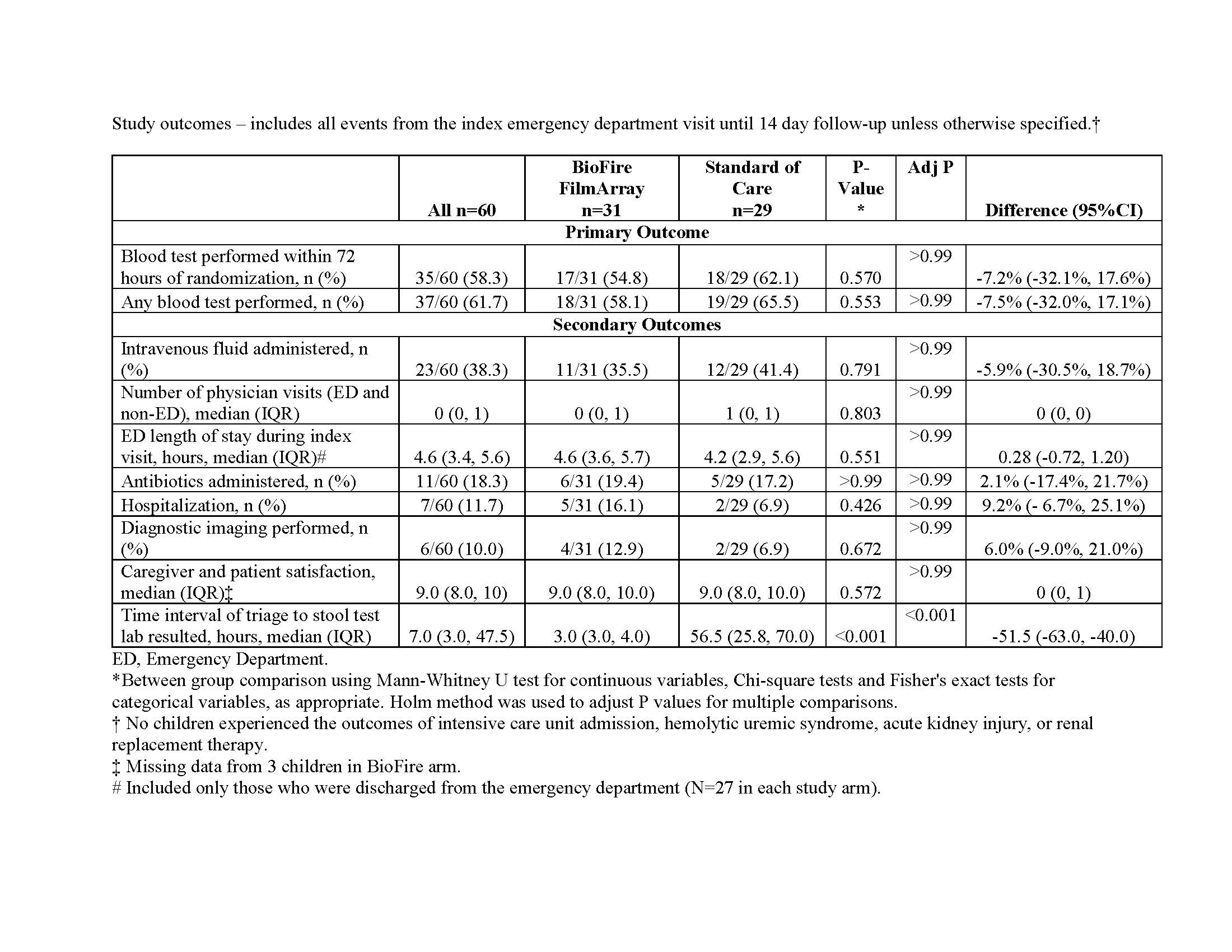
From June 2018, through May 2022, 60 children were enrolled and randomized. Patients in the Biofire arm had a shorter time to stool test result than the standard of care arm [median (IQR) 3 (3, 4) hours vs. 57 (26, 70) hours; difference -52 hours, 95%CI of difference: -63, -40)]. The pathogens most frequently identified using standard of care testing were Campylobacter spp. (20%, 11/56) and Salmonella spp. (9%, 5/56). Two participants had E coli O157:H7 identified, and one child had a non-O157 STEC detected. Sixty-five percent (20/31) participants in the BioFire FilmArray study group had a pathogen detected – most frequently enteropathogenic Escherichia coli (19%, 6/31), Campylobacter (16%, 5/31) and Salmonella (13%, 4/31). Blood tests were performed in 52% (16/31) of children in the BioFire and 62% (18/29) in the standard of care groups, difference: -11%; 95%CI of difference: -35%, 15%. There were no between group differences in the proportions of children administered intravenous fluids, antibiotics, hospitalized, or had diagnostic imaging performed.
Conclusion(s): Testing with the BioFire FilmArray Gastrointestinal Panel reduced the time to result availability by over 50 hours and identified a greater number of pathogens. Use however was not associated with a reduction in health care utilization, improved outcomes or greater patient/parent satisfaction.