Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 9
585 - Neighborhood opportunity and development of persistent wheeze/asthma in early childhood
Publication Number: 585.413

Jordan Tyris, MD, MSHS (she/her/hers)
Pediatric Hospital Medicine Fellow
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background:
The Child Opportunity Index (COI) incorporates 29 place-based characteristics organized into three domains (Educational, Health/Environmental, Social/Economic) to broadly describe a child’s neighborhood. Decreased COI, or less opportunity, is associated with increased pediatric asthma morbidity. While neighborhood poverty is associated with an increased risk of persistent wheeze, similar associations between the comprehensive COI and the development of persistent wheeze/asthma in early childhood have not been characterized.
Objective: To evaluate associations between COI at birth and development of persistent wheeze/asthma by 3 years of age.
Design/Methods:
Upstate KIDS is a prospective, population-based birth cohort from New York state designed to study the effects of fertility treatment on child health. Addresses were geocoded to census tracts and assigned COI data. Exposure variables were nationally-normed quintiles (very low, low, moderate, high, very high) of the COI and its three domains. The outcome variable was persistent wheeze ( >2 episodes of wheeze, assessed at 4, 8, 12, 18, 24, 30, and 36 months) and/or physician diagnosed asthma (assessed at 18, 24, 30, and 36 months) by 3 years of age. Data were compared using one-way ANOVA and chi square tests. Associations were analyzed with linear mixed models with a logit link and a random effect for infants nested within mothers (i.e., twins), adjusted for child sex, plurality, maternal smoking during pregnancy, fertility treatment, and parental history of asthma.
Results:
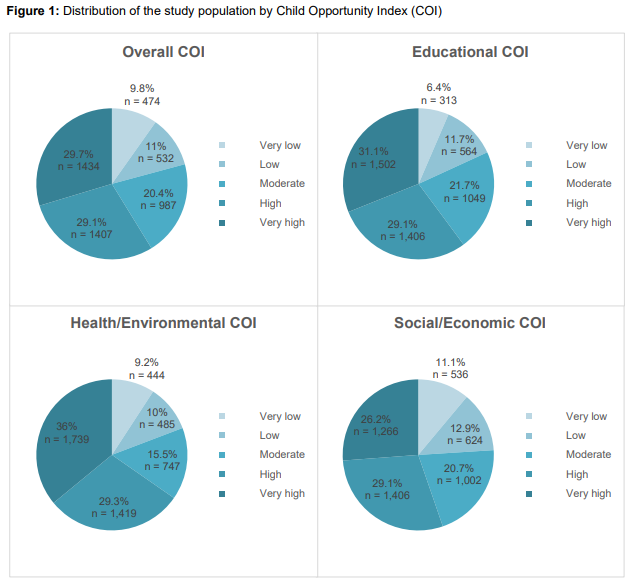
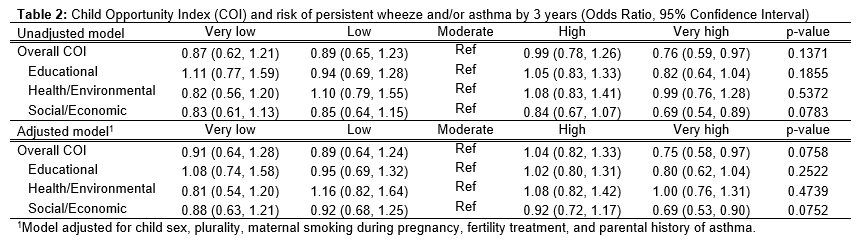
The study included 4,834 children, of whom 489 (10.1%) had persistent wheeze/asthma by the age of 3 years; these children were more likely to be male, conceived using fertility treatment, and have a parent with asthma (Table 1). Most children experienced very high (29.7%) or high (29.1%) overall COI compared to low (11%) or very low (9.8%) COI (Figure 1). While there was a reduced risk of developing persistent wheeze/asthma among children experiencing very high overall and Social/Economic COI compared to moderate COI at birth, no graded associations appeared between the COI and development of persistent wheeze/asthma (Table 2).
Conclusion(s):
In this prospective cohort of children experiencing higher neighborhood opportunity, COI at birth was generally not associated with the development of persistent wheeze/asthma in early childhood. Next, we will examine associations between the COI post birth and diagnosis of asthma at older age as well as individual social factors that may be effect modifiers..png)